
SURVEY BRIEF
FEBRUARY 2019
Health Insurance Coverage
Eight Years Aer the ACA:
Fewer Uninsured
Americans and
Shorter Coverage
Gaps, But More
Underinsured
Sara R. Collins
Vice President
The Commonwealth Fund
Herman K. Bhupal
Program Associate
The Commonwealth Fund
Michelle M. Doty
Vice President
The Commonwealth Fund
What does health insurance coverage look like for Americans today, more than eight
years aer the Aordable Care Act’s passage? In this brief, we present findings from the
Commonwealth Fund’s latest Biennial Health Insurance Survey to assess the extent
and quality of coverage for U.S. working-age adults. Conducted since 2001, the survey
uses three measures to gauge the adequacy of people’s coverage:
• whether or not they have insurance
• if they have insurance, whether they have experienced a gap in their coverage in
the prior year
• whether high out-of-pocket health care costs and deductibles are causing them to
be underinsured, despite having continuous coverage throughout the year.
As the findings highlighted below show, the greatest deterioration in the quality and
comprehensiveness of coverage has occurred among people in employer plans. More
than half of Americans under age 65 — about 158 million people — get their health
insurance through an employer, while about one-quarter either have a plan purchased
through the individual insurance market or are enrolled in Medicaid.
1
Although the
ACA has expanded and improved coverage options for people without access to a job-
based health plan, the law largely le the employer market alone.
2
SURVEY HIGHLIGHTS
Today, 45 percent of U.S. adults ages 19 to 64 are inadequately insured — nearly the
same as in 2010 — though important shis have taken place.
Compared to 2010, many fewer adults are uninsured today, and the duration of
coverage gaps people experience has shortened significantly.
Despite actions by the Trump administration and Congress to weaken the ACA, the
adult uninsured rate was 12.4 percent in 2018 in this survey, statistically unchanged
from the last time we fielded the survey in 2016
.
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 2
More people who have coverage are underinsured now than
in 2010, with the greatest increase occurring among those in
employer plans.
People who are underinsured or spend any time uninsured
report cost-related problems getting care and diculty paying
medical bills at higher rates than those with continuous,
adequate coverage.
Federal and state governments could enact policies to extend
the ACA’s health coverage gains and improve the cost protection
provided by individual-market and employer plans.
The 2018 Commonwealth Fund Biennial Heath Insurance Survey
included a nationally representative sample of 4,225 adults ages 19
to 64. SSRS conducted the telephone survey between June 27 and
November 11, 2018.
3
(See “How We Conducted This Study” for more
detail.)
WHO IS UNDERINSURED?
In this analysis, we use a measure of underinsurance that accounts
for an insured adult’s reported out-of-pocket costs over the course
of a year, not including insurance premiums, as well as his or her plan
deductible. (The measure was first used in the Commonwealth Fund’s
2003 Biennial Health Insurance Survey.*) These actual expenditures
and the potential risk of expenditures, as represented by the deductible,
are then compared with household income. Specifically, we consider
people who are insured all year to be underinsured if:
• their out-of-pocket costs, excluding premiums, over
the prior 12 months are equal to 10 percent or more of
household income; or
• their out-of-pocket costs, excluding premiums, over
the prior 12 months are equal to 5 percent or more of
household income for individuals living under 200 percent
of the federal poverty level ($24,120 for an individual or
$49,200 for a family of four); or
• their deductible constitutes 5 percent or more of
household income.
The out-of-pocket cost component of the measure is only triggered
if a person uses his or her plan to obtain health care. The deductible
component provides an indicator of the financial protection the plan
offers and the risk of incurring costs before someone gets health
care. The definition does not include other dimensions of someone’s
health plan that might leave them potentially exposed to costs, such as
copayments or uncovered services. It therefore provides a conservative
measure of underinsurance in the United States.
* Cathy Schoen et al., “Insured But Not Protected: How Many Adults Are Underinsured?” Health
Affairs Web Exclusive, published online June 14, 2005.
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 3
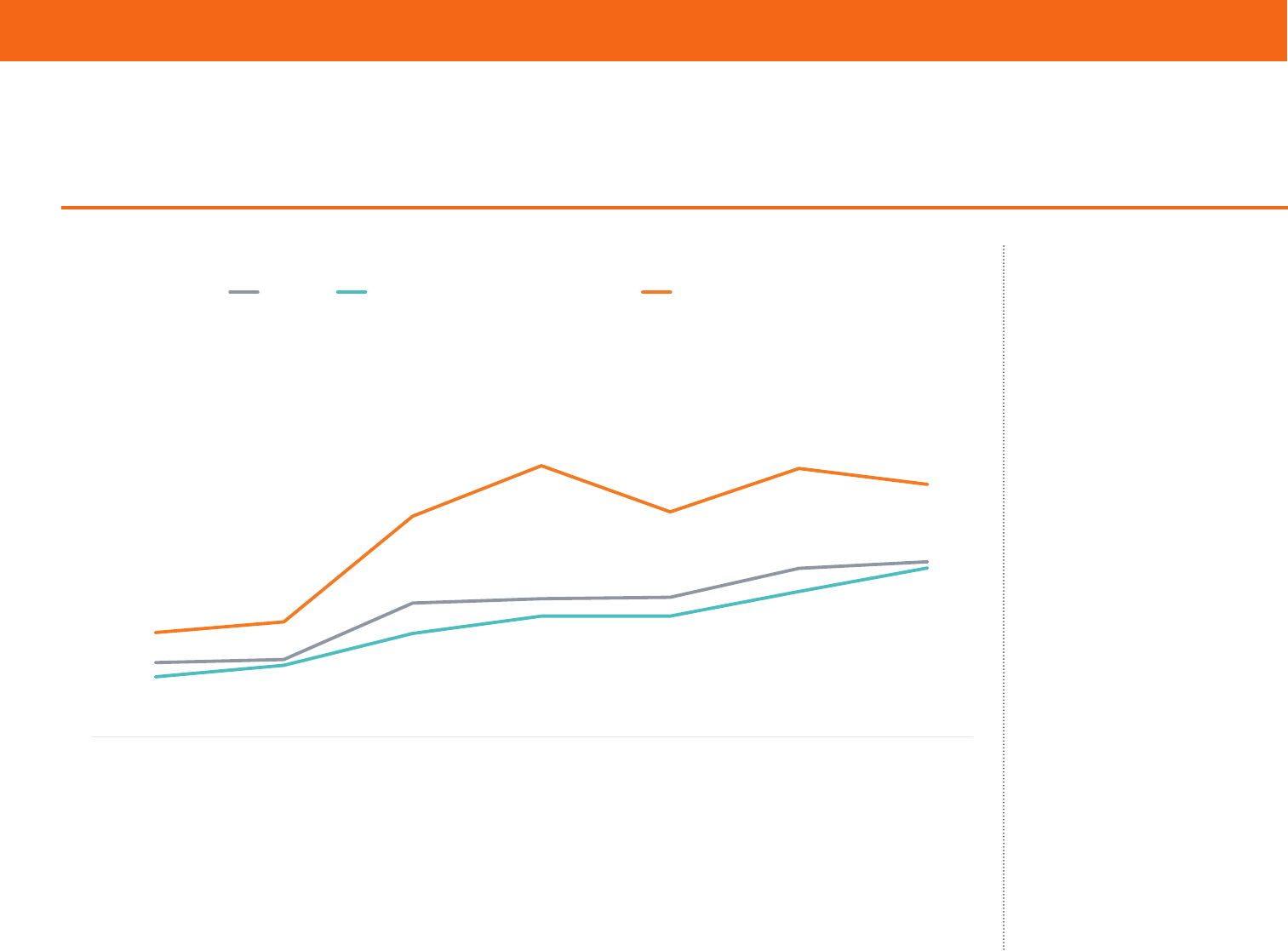
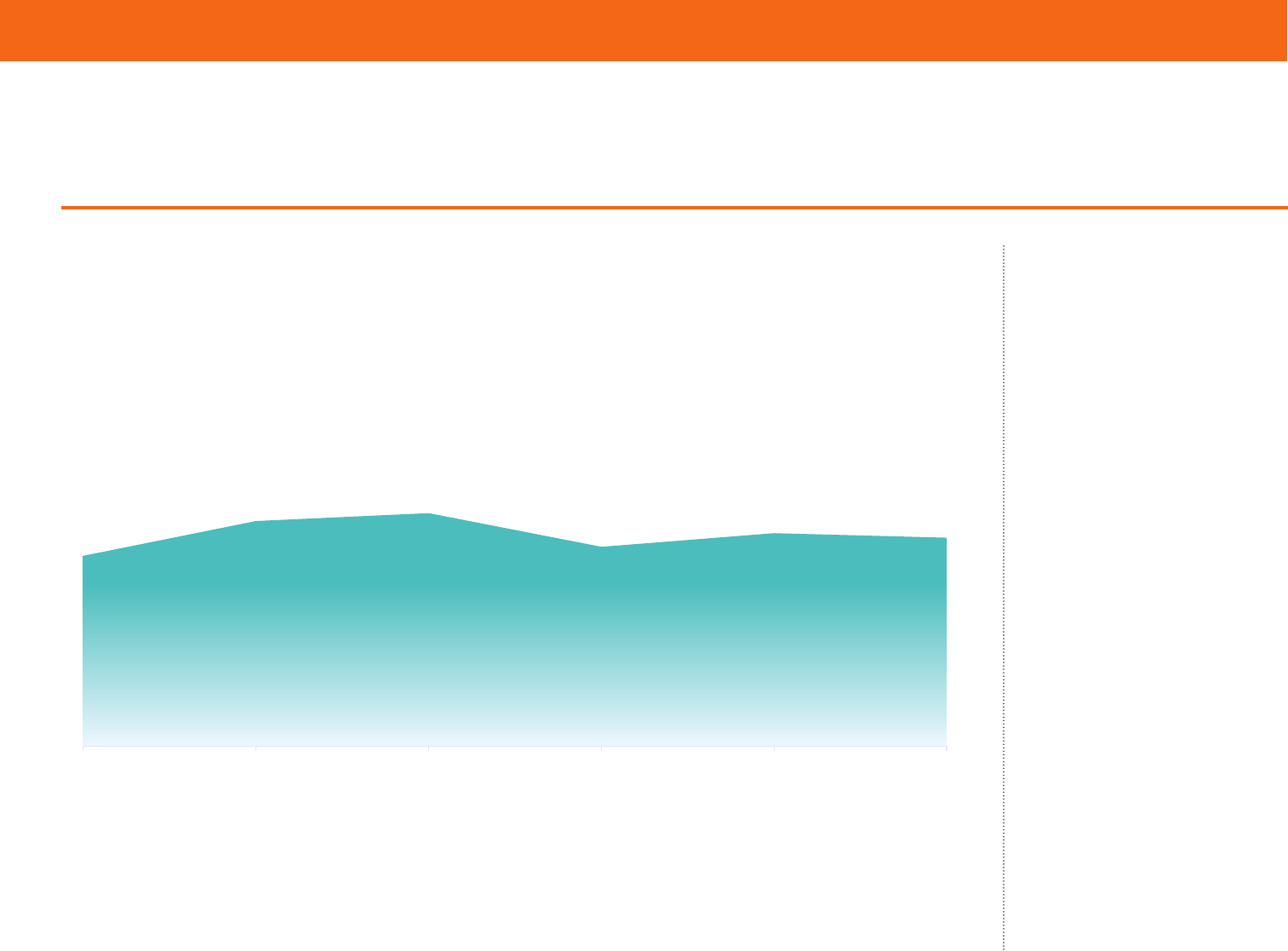
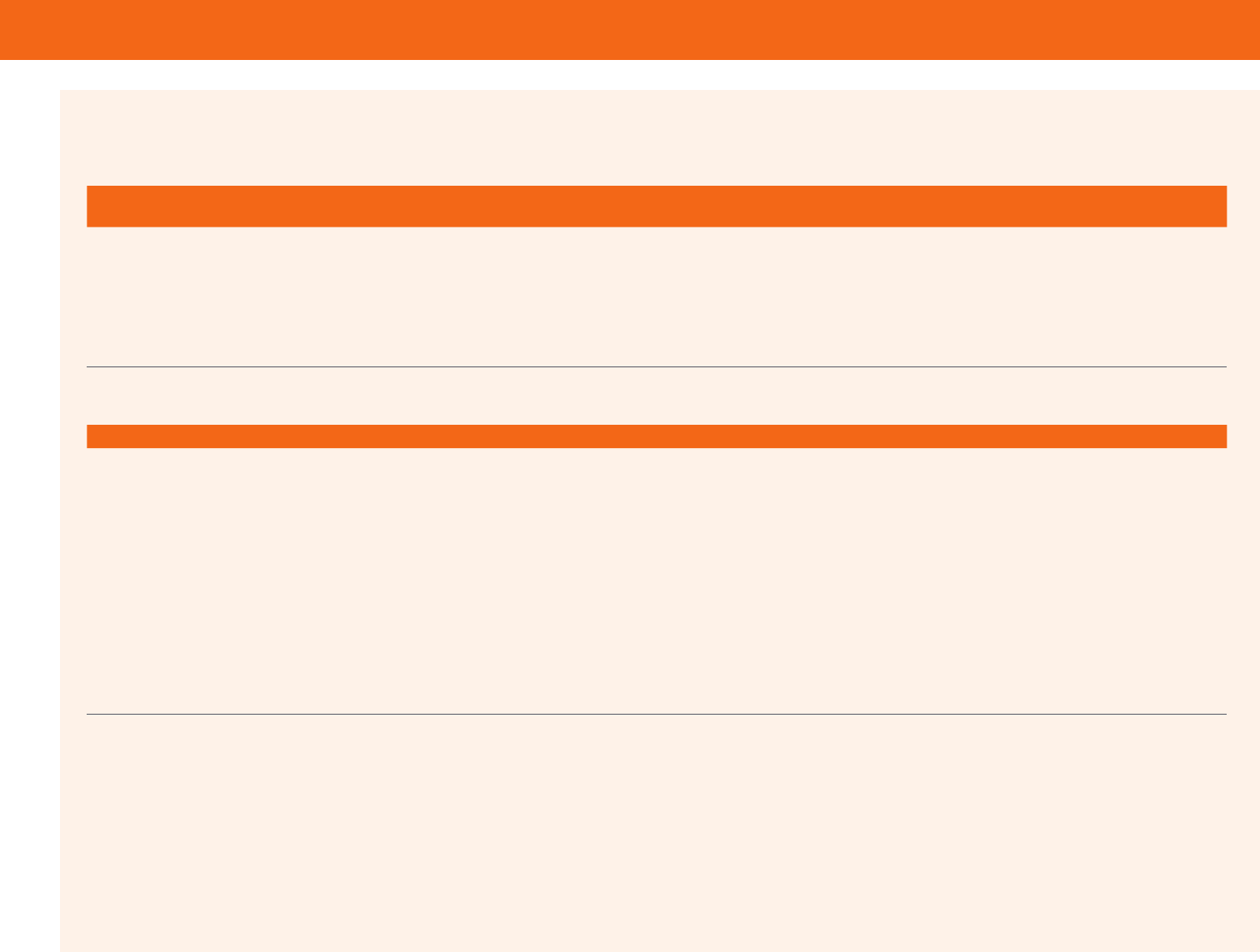
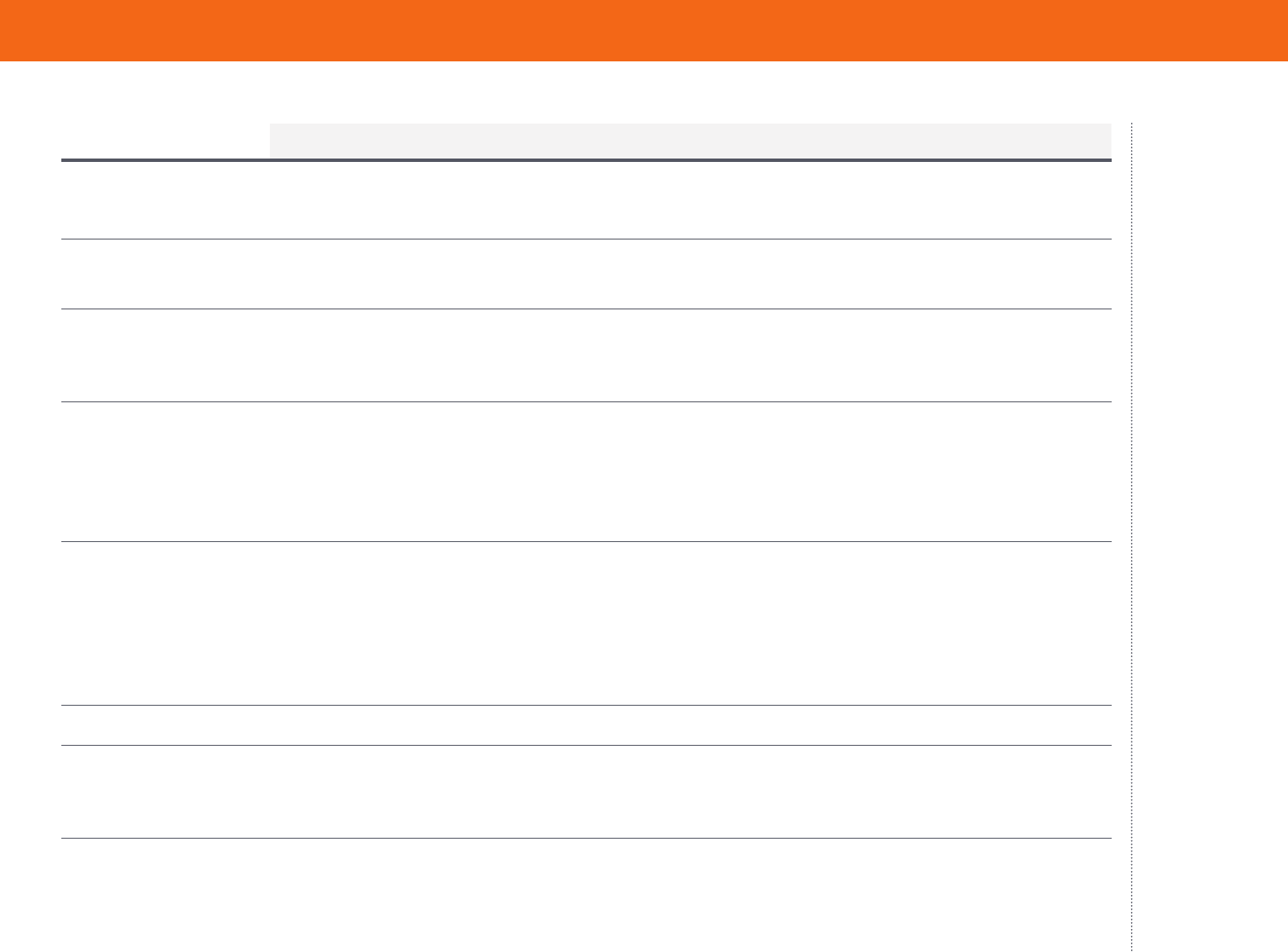
Source: Sara R. Collins, Herman K. Bhupal, and Michelle M. Doty, Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and
Shorter Coverage Gaps, But More Underinsured — Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2018 (Commonwealth Fund,
Feb. 2019).
17%
18%
20%
19%
16%
12%
12%
9%
9%
8%
10%
13%
10%
10%
9%
9%
16%
16%
17%
22%
23%
65%
63%
56%
54% 55%
56%
55%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
2003 2005 2010 2012 2014 2016 2018
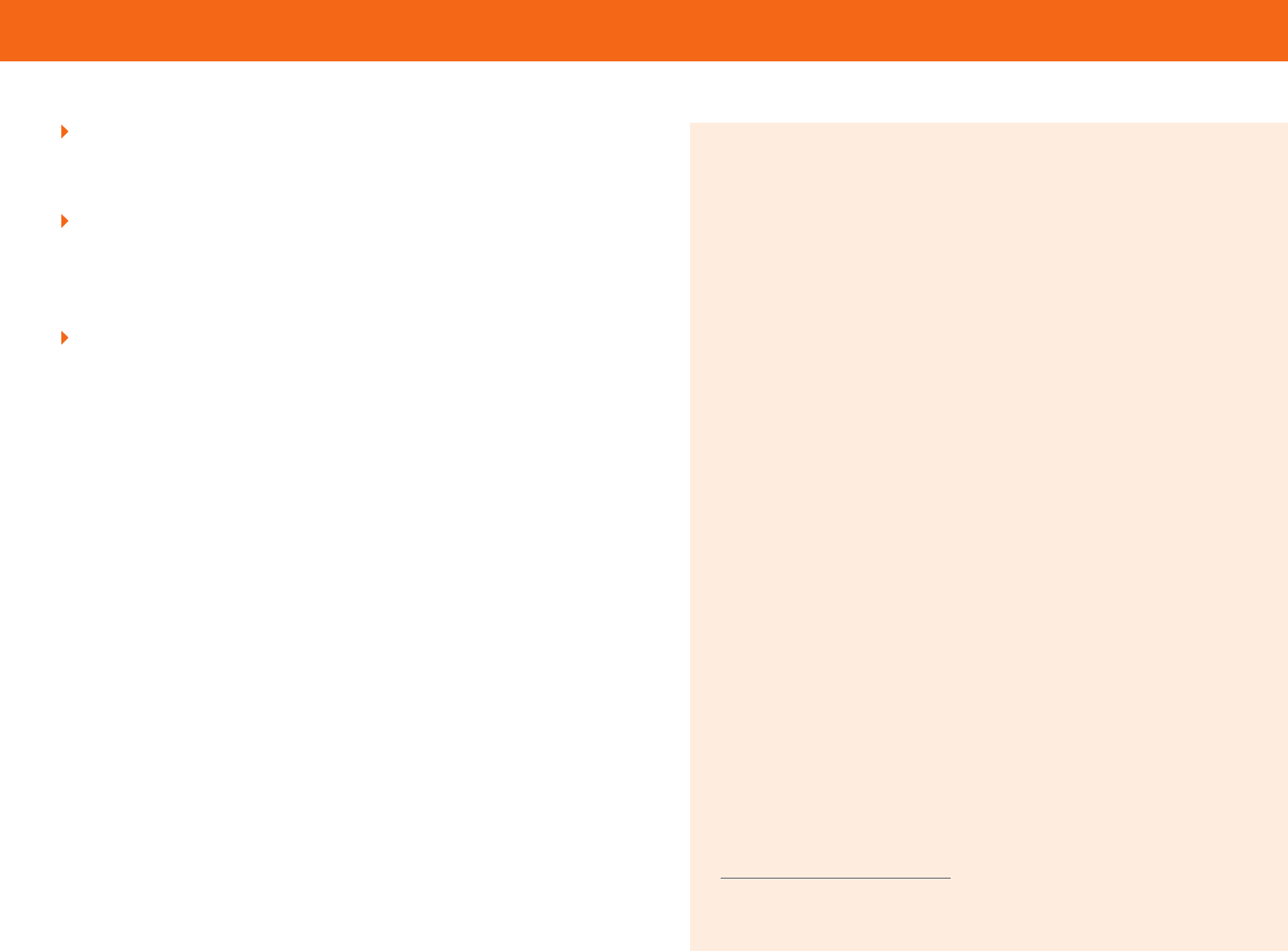
Since the ACA, Fewer Adults Are Uninsured, but More Are Underinsured
Percent of adults ages 19–64
Notes: “Underinsured” refers to adults who were insured all year but experienced one of the following: out-of-pocket costs, excluding premiums, equaled 10% or more of income; out-of-pocket costs,
excluding premiums, equaled 5% or more of income if low-income (<200% of poverty); or deductibles equaled 5% or more of income. “Insured now, had a coverage gap” refers to adults who were
insured at the time of the survey but were uninsured at any point in the 12 months prior to the survey field date. “Uninsured now” refers to adults who reported being uninsured at the time of the
survey.
Data: Commonwealth Fund Biennial Health Insurance Surveys (2003, 2005, 2010, 2012, 2014, 2016, 2018).
Insured all year, not underinsured
Insured now, had a coverage gap
Insured all year, underinsured
Uninsured now
Notes: “Underinsured” refers to adults who were insured all year but experienced one of the following: out-of-pocket costs, excluding
premiums, equaled 10% or more of income; out-of-pocket costs, excluding premiums, equaled 5% or more of income if low-income (<200%
of poverty); or deductibles equaled 5% or more of income. “Insured now, had a coverage gap” refers to adults who were insured at the time of
the survey but were uninsured at any point in the 12 months prior to the survey eld date. “Uninsured now” refers to adults who reported being
uninsured at the time of the survey.
Data: Commonwealth Fund Biennial Health Insurance Surveys (2003, 2005, 2010, 2012, 2014, 2016, 2018).
Since the ACA, Fewer Adults Are Uninsured, but More Are Underinsured
Compared to 2010, when
the ACA became law, fewer
people today are uninsured,
but more people are
underinsured. Of the 194
million U.S. adults ages 19 to
64 in 2018, an estimated 87
million, or 45 percent, were
inadequately insured (see
Tables 1 and 2).
Despite actions by the
Trump administration and
Congress to weaken the
ACA, our survey found no
statistically significant change
in the adult uninsured rate
by late 2018 compared to
2016 (Table 3). This finding
is consistent with recent
federal surveys, but other
private surveys (including
other Commonwealth Fund
surveys) have found small
increases in uninsured rates
since 2016 (see Changes in U.S.
Uninsured Rates Since 2013).
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 4
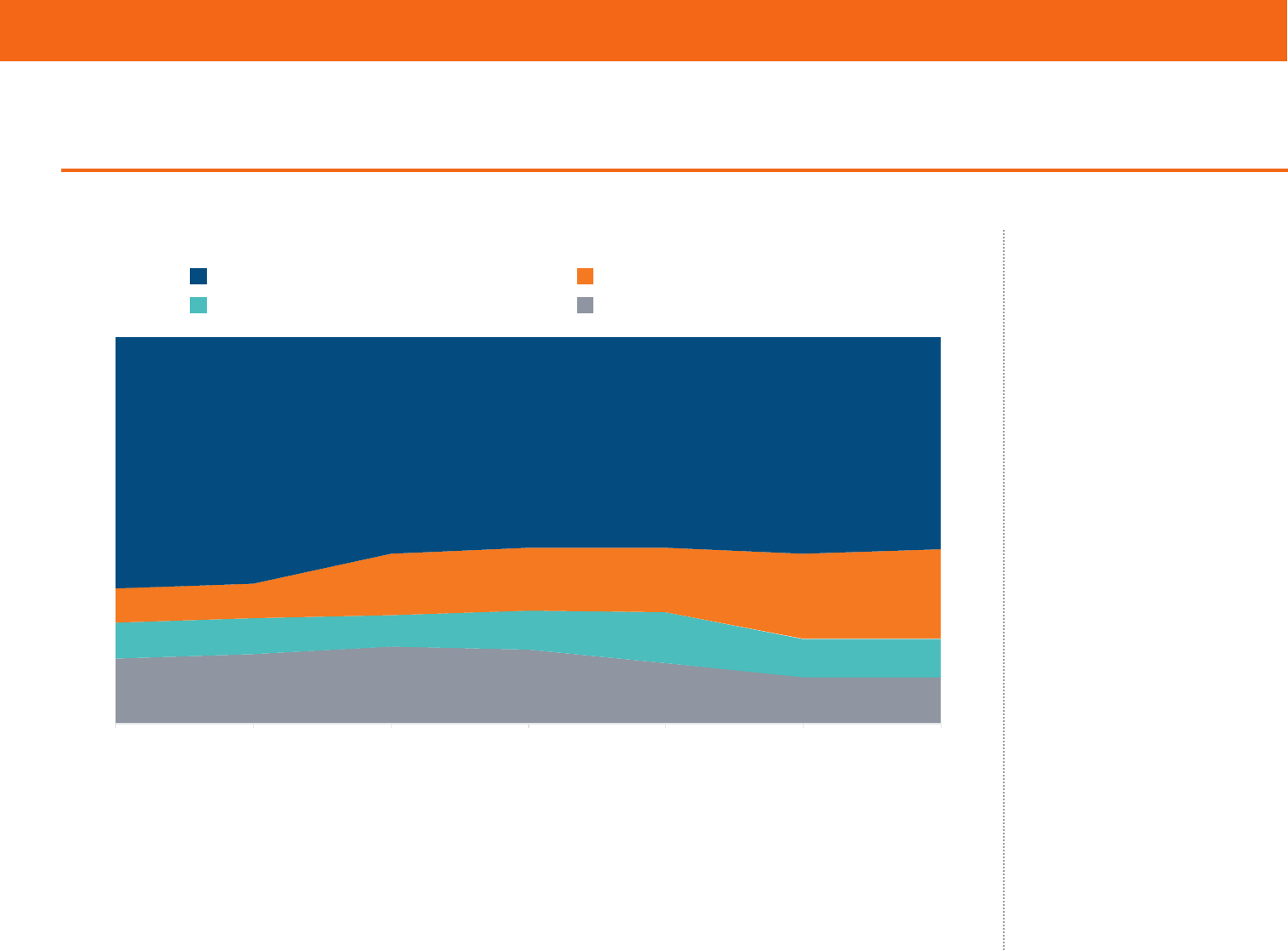
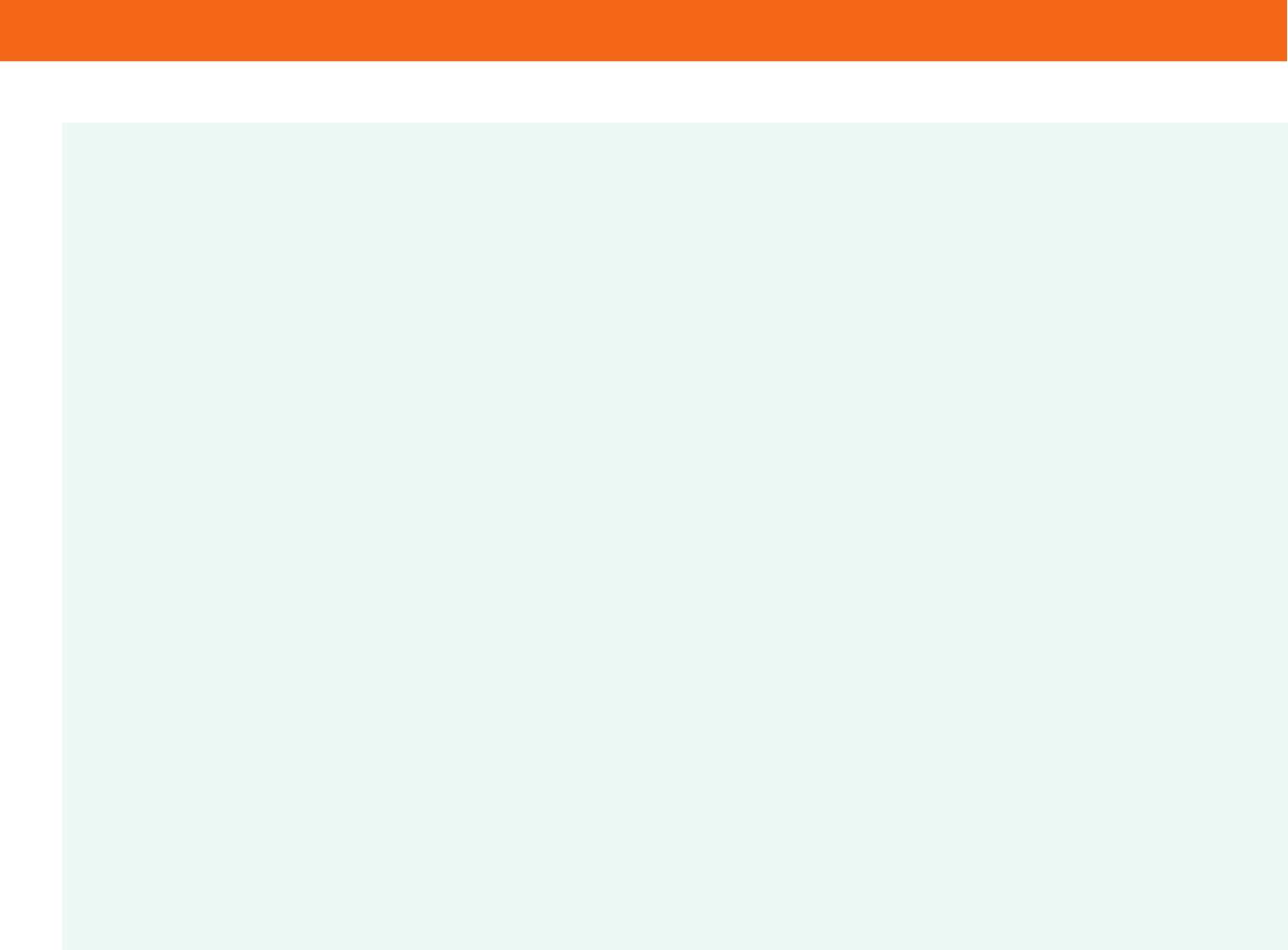
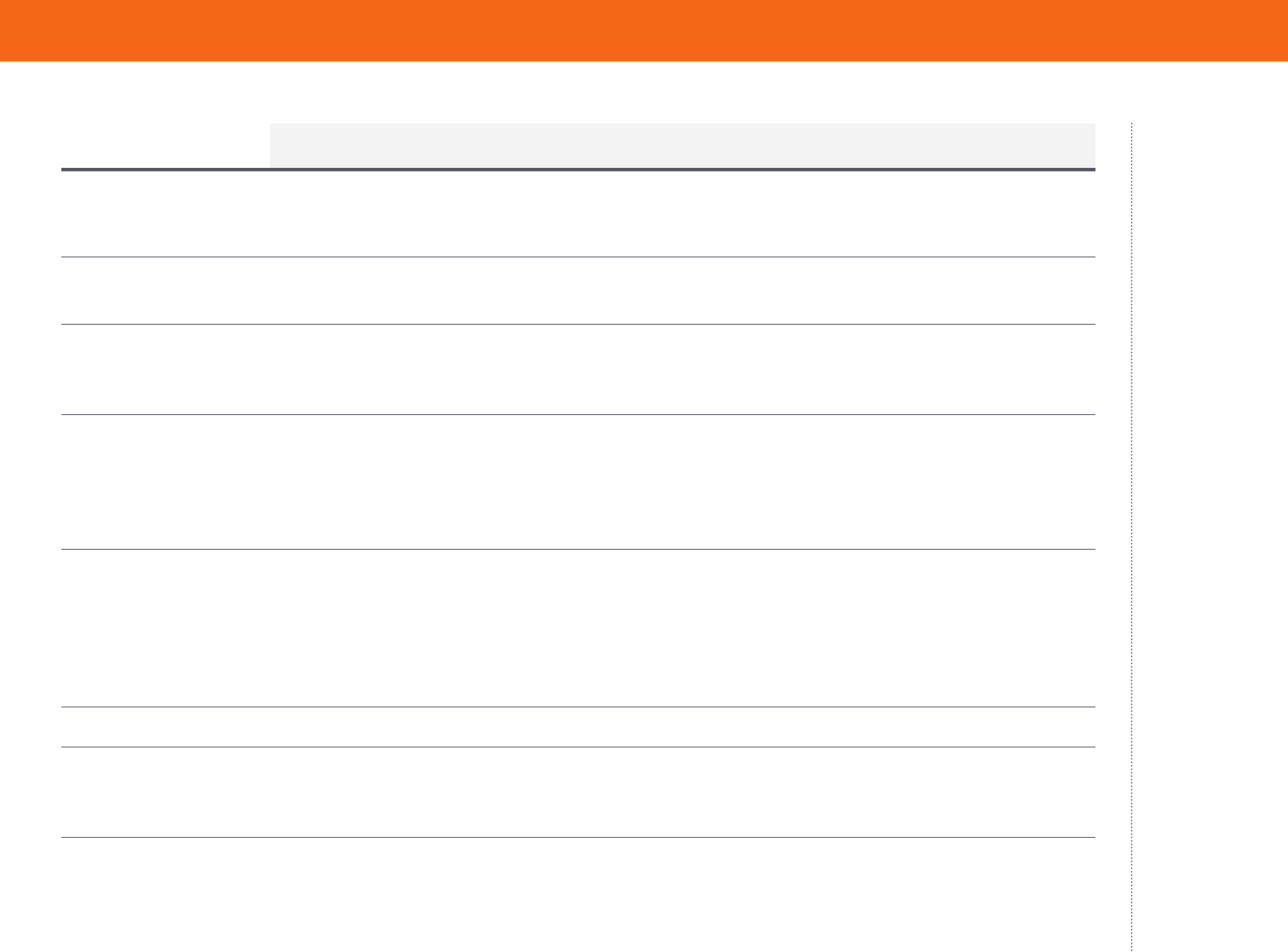
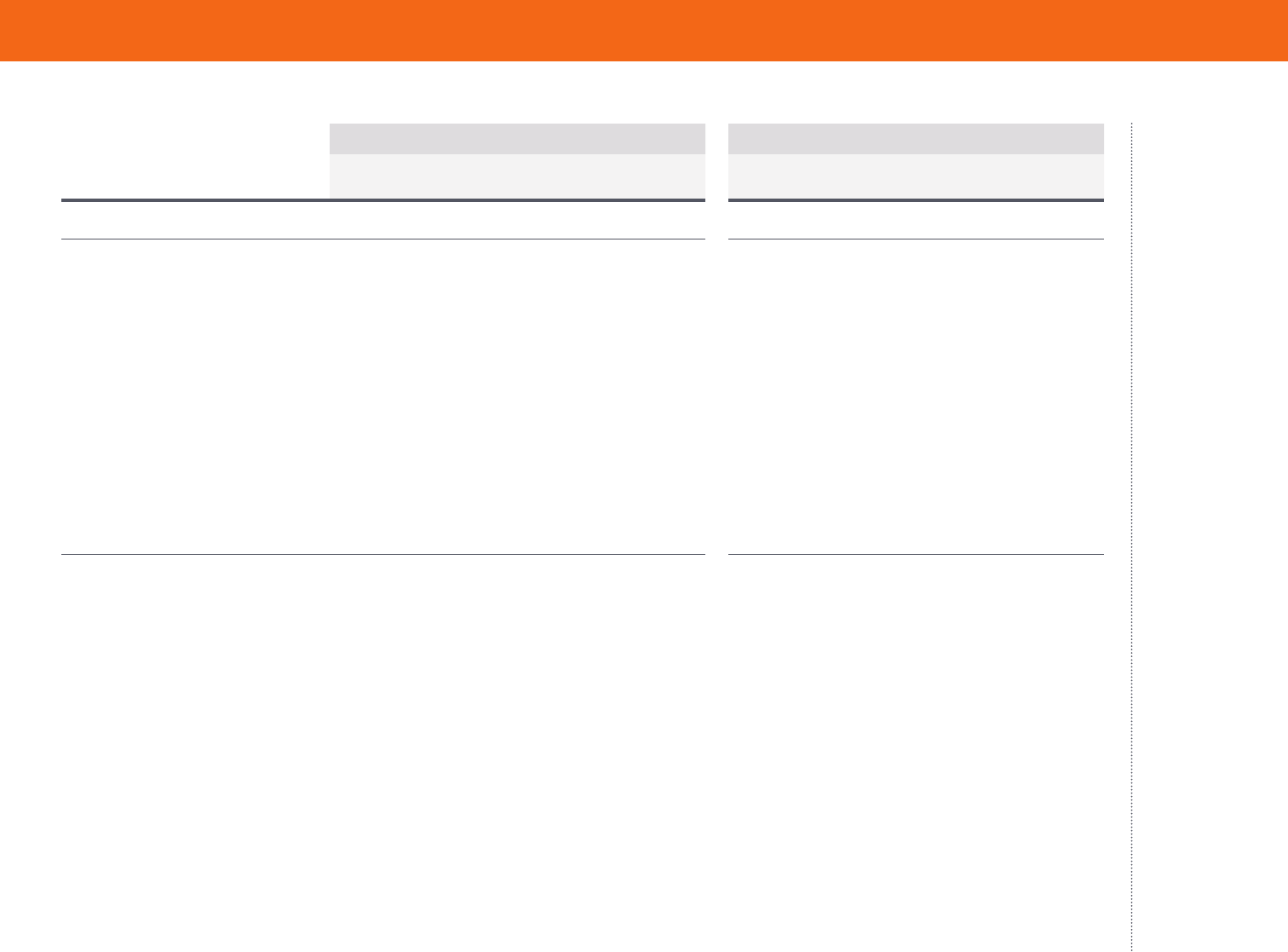
Since the ACA, Gaps in People’s Coverage Have Been Shorter
Data: Commonwealth Fund Biennial Health Insurance Surveys (2001, 2010, 2012, 2014, 2016, 2018).
While there has been
no change since 2010,
statistically speaking, in
the proportion of people
who are insured now but
have experienced a recent
time without coverage,
these reported gaps are
of much shorter duration
on average than they were
before the ACA. In 2018,
61 percent of people who
reported a coverage gap said
it has lasted for six months
or less, compared to 31
percent who said they had
been uninsured for a year
or longer. This is nearly a
reverse of what it was like
in 2012, two years before
the ACA’s major coverage
expansions. In that year,
57 percent of adults with
a coverage gap reported
it was for a year or longer,
while one-third said it was a
shorter gap.
Source: Sara R. Collins, Herman K. Bhupal, and Michelle M. Doty, Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and
Shorter Coverage Gaps, But More Underinsured — Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2018 (Commonwealth Fund,
Feb. 2019).
Since the ACA, Gaps in People’s Coverage Have Been Shorter
65
47
35
38
54
61
25
39
57
55
38
31
0
10
20
30
40
50
60
70
80
2001 2010 2012 2014 2016 2018
Coverage gap of 6 months or less Coverage gap of 1 year or more
Percent of adults ages 19–64 insured now but had a coverage gap in past year
Data: Commonwealth Fund Biennial Health Insurance Surveys (2001, 2010, 2012, 2014, 2016, 2018).
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 5
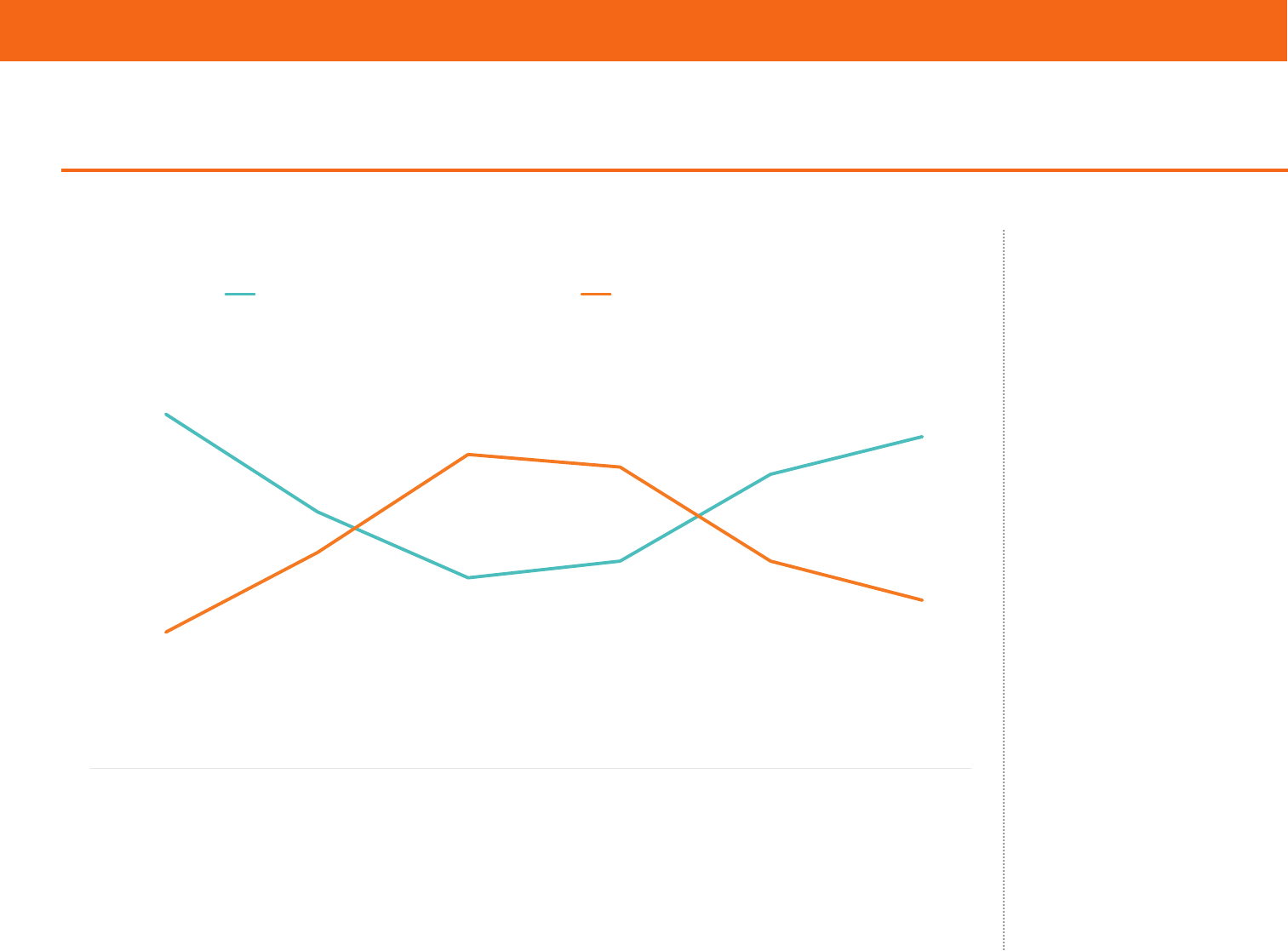
There Has Been Some Improvement in Long-Term Uninsured Rates
There also has been some
improvement in long-term
uninsured rates. Among
adults who were uninsured
at the time of the survey, 54
percent reported they had
been without coverage for
more than two years, down
from 72 percent before the
ACA coverage expansions
went into eect. The share
of those who had been
uninsured for six months or
less climbed to 20 percent,
nearly double the rate prior
to the coverage expansions.
Data: Commonwealth Fund Biennial Health Insurance Surveys (2001, 2010, 2012, 2014, 2016, 2018).
Source: Sara R. Collins, Herman K. Bhupal, and Michelle M. Doty, Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and
Shorter Coverage Gaps, But More Underinsured — Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2018 (Commonwealth Fund,
Feb. 2019).
There Has Been Some Improvement in Long-Term Uninsured Rates
19
11
12
13
21
20
62
63
72
64
53
54
0
10
20
30
40
50
60
70
80
2001 2010 2012 2014 2016 2018
Uninsured for 6 months or less Uninsured for more than 2 years
Data: Commonwealth Fund Biennial Health Insurance Surveys (2001, 2010, 2012, 2014, 2016, 2018).
Percent of adults ages 19–64 who are uninsured now
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 6
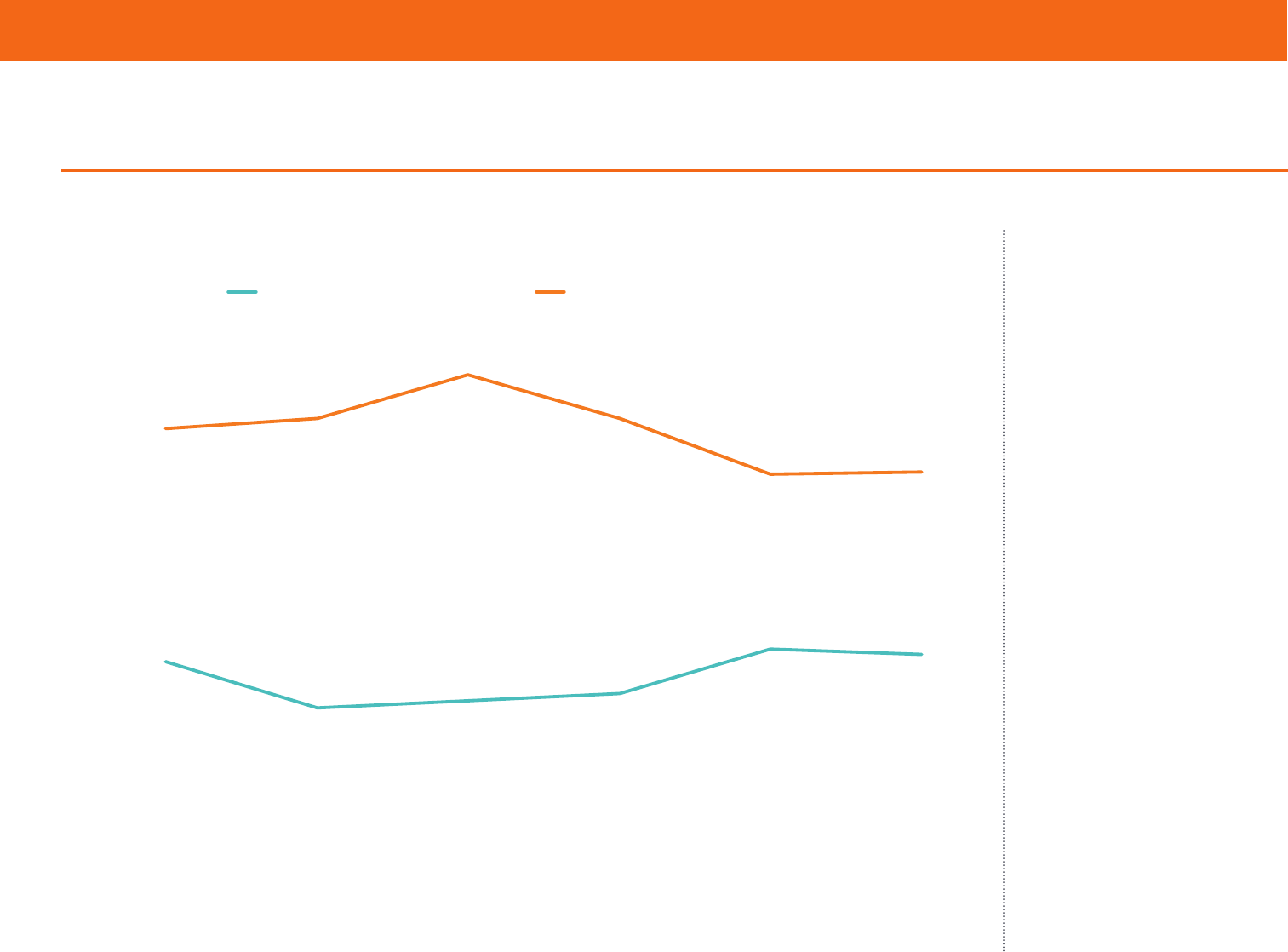
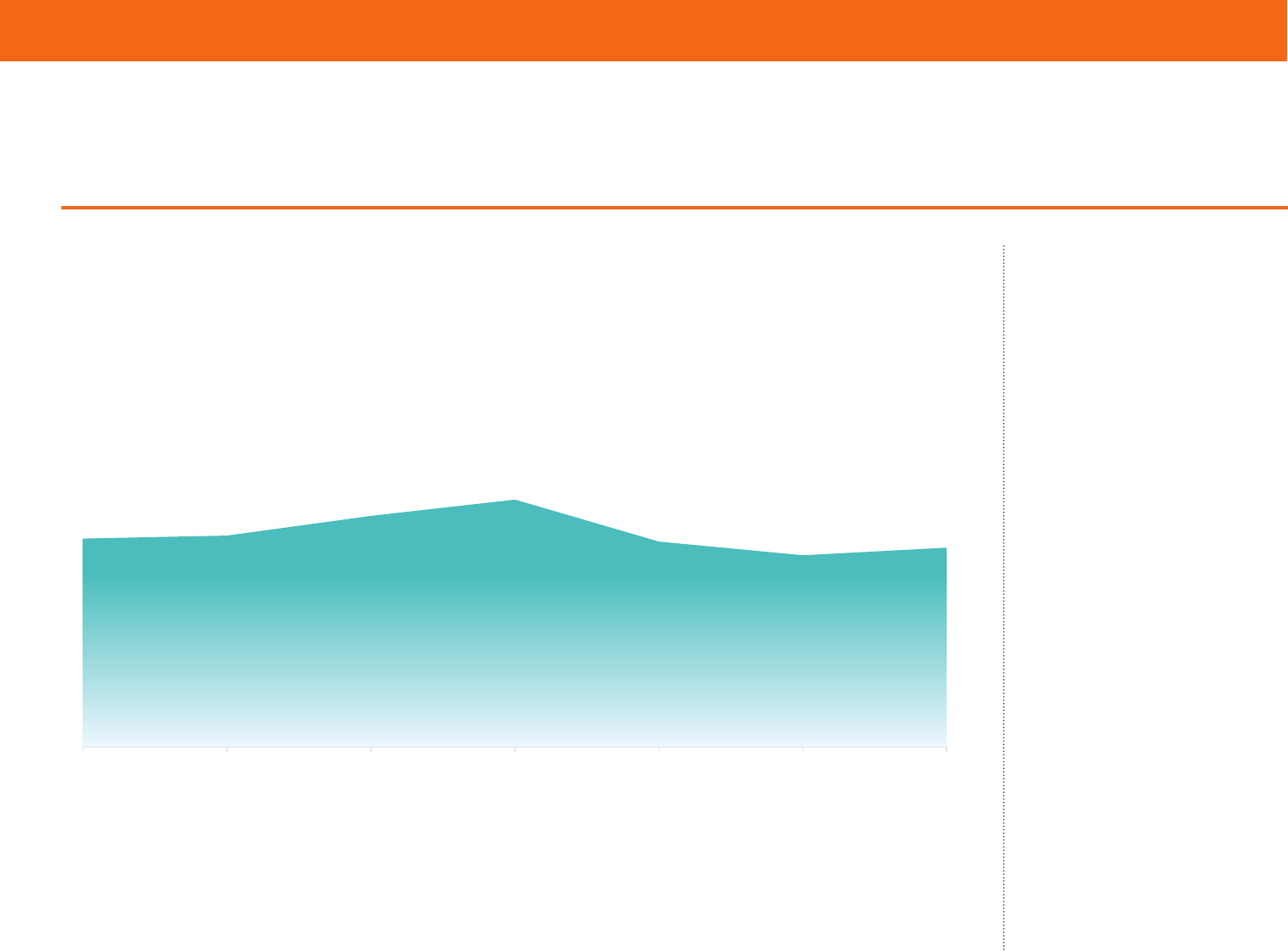
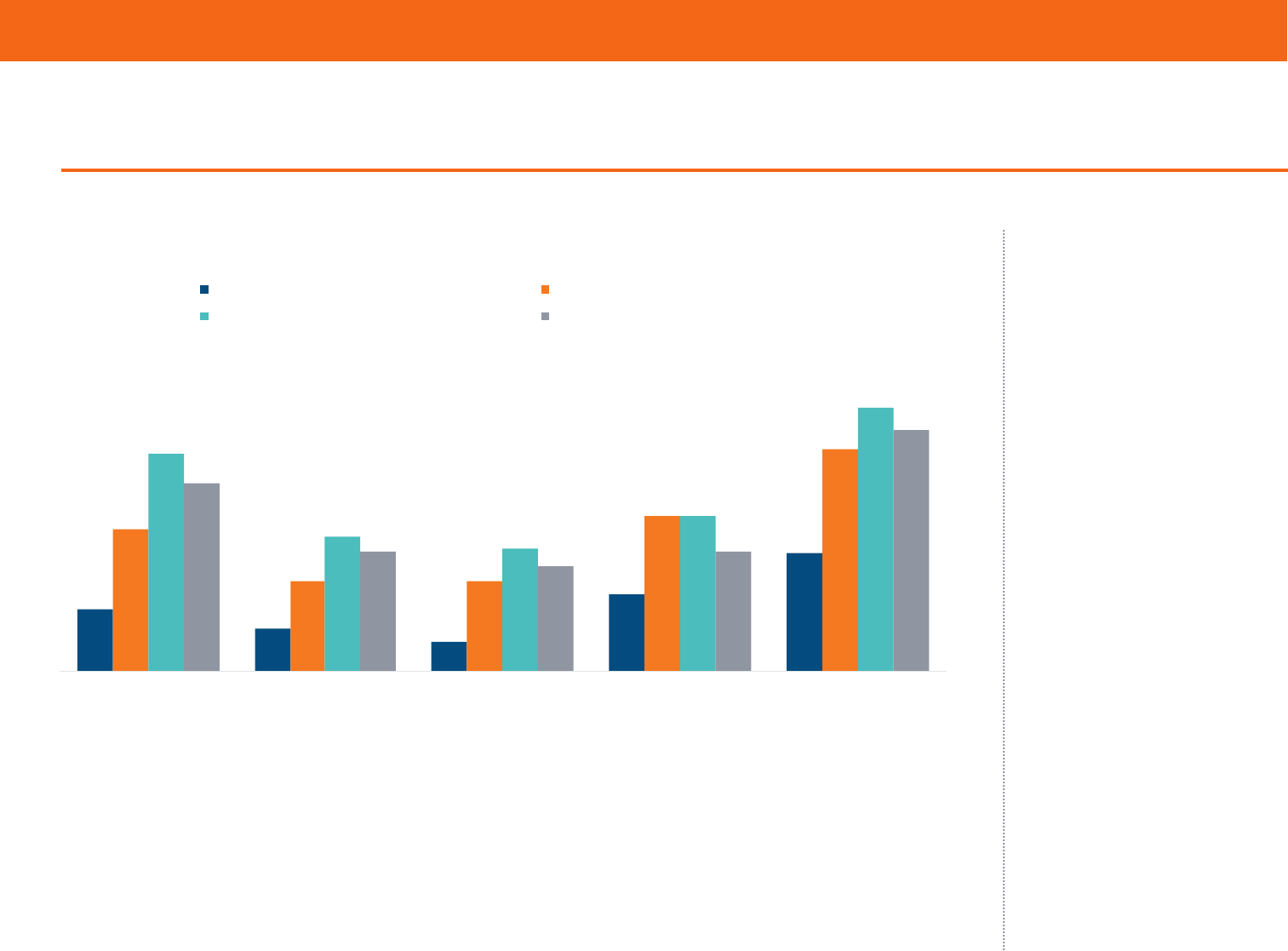
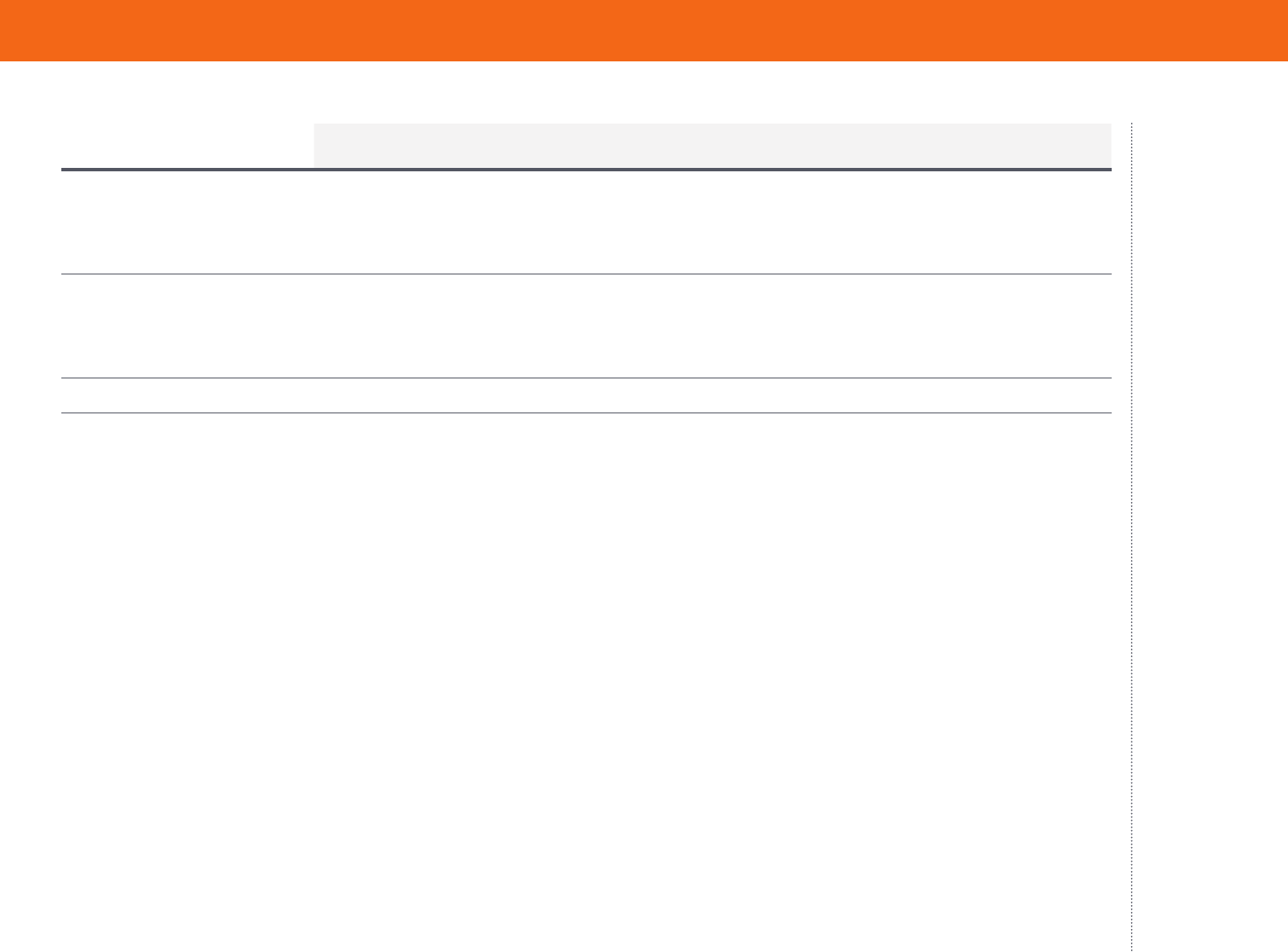
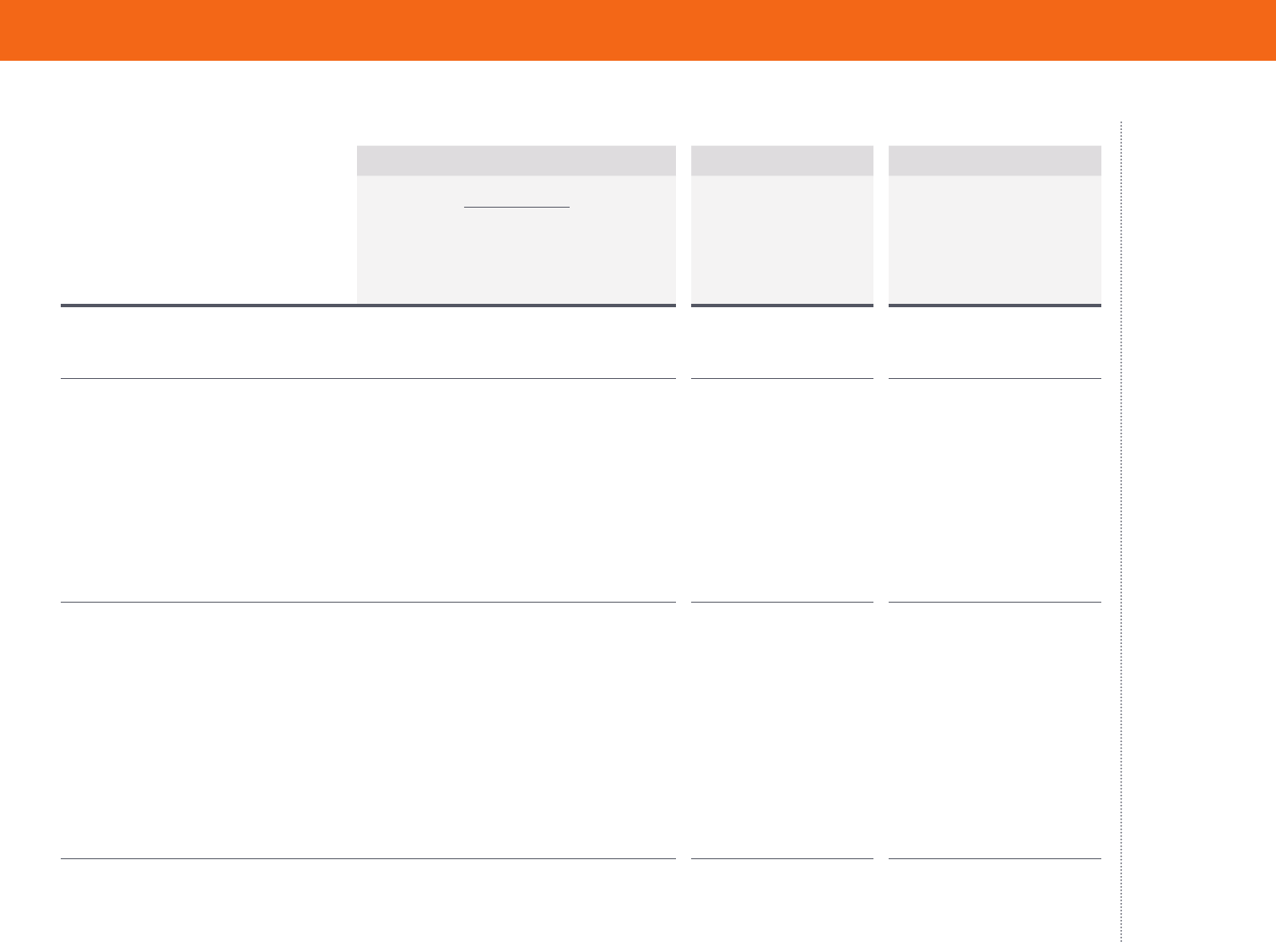
More Adults Are Underinsured, with the Greatest Growth Occurring Among Those
with Employer Coverage
Notes: “Underinsured” refers to adults who were insured all year but experienced one of the following: out-of-pocket costs, excluding
premiums, equaled 10% or more of income; out-of-pocket costs, excluding premiums, equaled 5% or more of income if low-income (<200% of
poverty); or deductibles equaled 5% or more of income. Total includes adults with coverage through Medicaid and Medicare. Respondents may
have had another type of coverage at some point during the year, but had coverage for the entire previous 12 months. ^ For 2014 and 2016,
includes those who get their individual coverage through the marketplace and outside of the marketplace.
Data: Commonwealth Fund Biennial Health Insurance Surveys (2003, 2005, 2010, 2012, 2014, 2016, 2018).
Of people who were insured
continuously throughout
2018, an estimated 44 million
were underinsured because
of high out-of-pocket costs
and deductibles (Table 1).
This is up from an estimated
29 million in 2010 (data
not shown). The most
likely to be underinsured
are people who buy plans
on their own through the
individual market including
the marketplaces. However,
the greatest growth in the
number of underinsured
adults is occurring among
those in employer health
plans.
Source: Sara R. Collins, Herman K. Bhupal, and Michelle M. Doty, Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and
Shorter Coverage Gaps, But More Underinsured — Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2018 (Commonwealth Fund,
Feb. 2019).
More Adults Are Underinsured, with the Greatest Growth Occurring Among Those with
Employer Coverage
Notes: “Underinsured” refers to adults who were insured all year but experienced one of the following: out-of-pocket costs, excluding premiums, equaled 10% or more of income; out-of-pocket costs,
excluding premiums, equaled 5% or more of income if low-income (<200% of poverty); or deductibles equaled 5% or more of income. Total includes adults with coverage through Medicaid and
Medicare. Respondents may have had another type of coverage at some point during the year, but had coverage for the entire previous 12 months. ^ For 2014 and 2016, includes those who get their
individual coverage through the marketplace and outside of the marketplace.
Data: Commonwealth Fund Biennial Health Insurance Surveys (2003, 2005, 2010, 2012, 2014, 2016, 2018).
12
13
22
23
23
28
29
10
12
17
20
20
24
28
17
19
37
45
37
44
42
0
10
20
30
40
50
60
70
2003 2005 2010 2012 2014 2016 2018
Total Employer-provided coverage Individual coverage^
Percent of adults ages 19–64 insured all year who were underinsured
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 7
Why Are Insured Americans Spending So Much of Their Income
on Health Care Costs?
Several factors may be contributing to high underinsured rates among adults in individual market plans and rising
rates in employer plans:
1. Although the Aordable Care Act’s reforms to the
individual market have provided consumers with greater
protection against health care costs, many moderate-
income Americans have not seen gains. The ACA’s essential
health benefits package, cost-sharing reductions for lower-
income families, and out-of-pocket cost limits have helped
make health care more aordable for millions of Americans.
But while the cost-sharing reductions have been particularly
important in lowering deductibles and copayments for
people with incomes under 250 percent of the poverty level
(about $62,000 for a family of four), about half of people who
purchase marketplace plans, and all of those buying plans
directly from insurance companies, do not have them.
4
2. The bans against insurers excluding people from
coverage because of a preexisting condition and rating
based on health status have meant that individuals with
greater health needs, and thus higher costs, are now
able to get health insurance in the individual market.
Not surprisingly, the survey data show that people with
individual market coverage are somewhat more likely to have
health problems than they were in 2010, which means they
also have higher costs.
3. While plans in the employer market historically have
provided greater cost protection than plans in the
individual market, businesses have tried to hold down
premium growth by asking workers to shoulder an
increasing share of health costs, particularly in the
form of higher deductibles.
5
While the ACA’s employer
mandate imposed a minimum coverage requirement on large
companies, the requirement amounts to just 60 percent of
typical person’s overall costs. This leaves the potential for
high plan deductibles and copayments.
4. Growth in Americans’ incomes has not kept pace with
growth in health care costs. Even when health costs rise
more slowly, they can take an increasingly larger bite out of
incomes.
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 8
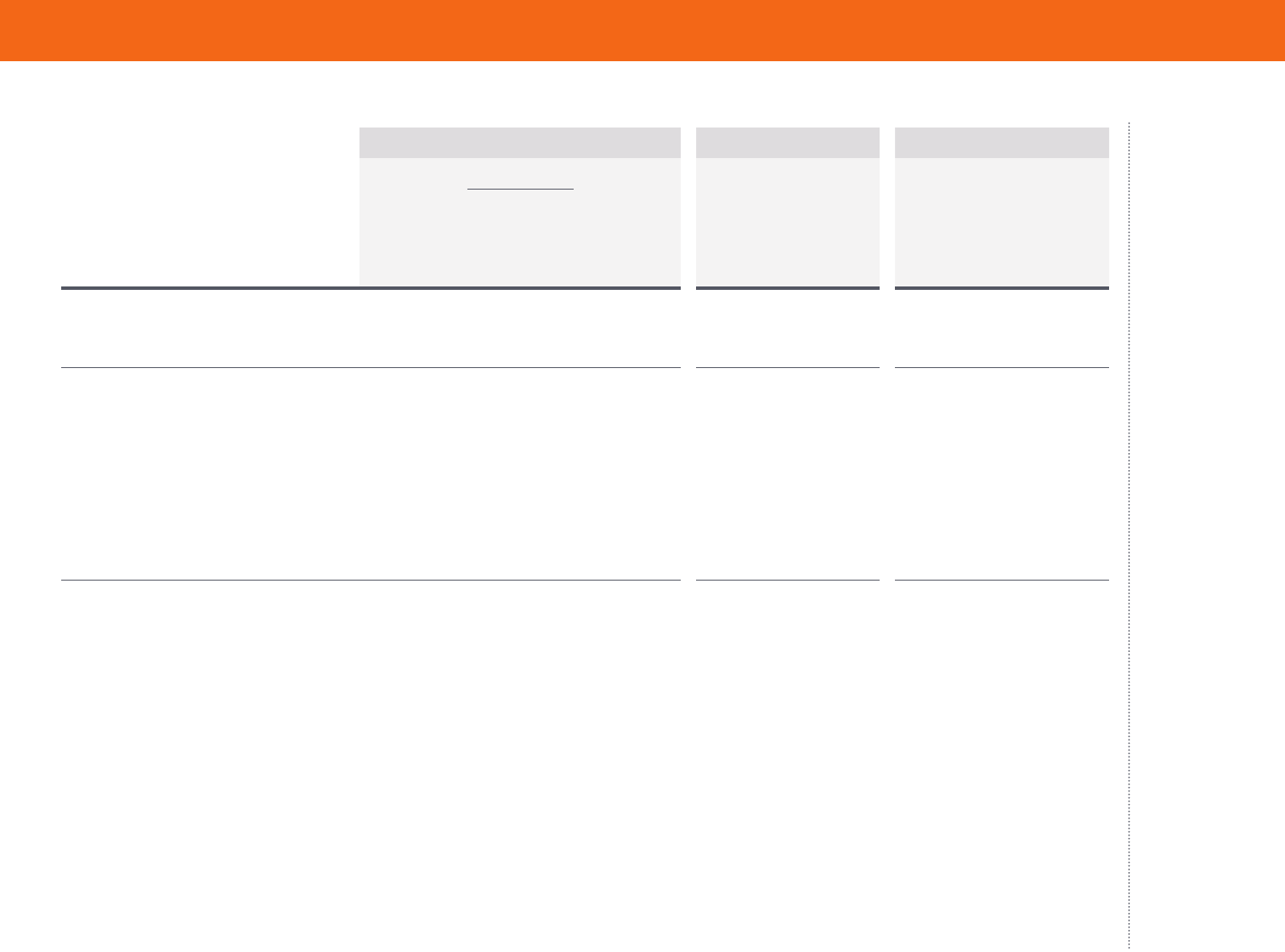
Fewer Adults Report Not Getting Needed Care Because of Costs, but Gains Have
Stalled in Recent Years
It is well documented that
people who gained coverage
under the ACA’s expansions
have better access to health
care as a result.
6
This has
led to overall improvement
in health care access, as
indicated by multiple
surveys.
7
In 2014, the year
the ACA’s major coverage
expansions went into
eect, the share of adults
in our survey who said
that cost prevented them
from getting health care
that they needed, such as
prescription medication,
dropped significantly (Table
4). But there has been no
significant improvement
since then.
Data: Commonwealth Fund Biennial Health Insurance Surveys (2003, 2005, 2010, 2012, 2014, 2016, 2018).
Source: Sara R. Collins, Herman K. Bhupal, and Michelle M. Doty, Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and
Shorter Coverage Gaps, But More Underinsured — Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2018 (Commonwealth Fund,
Feb. 2019).
Fewer Adults Report Not Getting Needed Care Because of Costs, but Gains Have Stalled in
Recent Years
Data: Commonwealth Fund Biennial Health Insurance Surveys (2003, 2005, 2010, 2012, 2014, 2016, 2018).
37
37
41
43
36
34
35
2003 2005 2010 2012 2014 2016 2018
Percent of adults ages 19–64 who reported any of the following
cost-related access problems in the past year:
• Had a medical problem but did not visit doctor or clinic
• Did not fill a prescription
• Skipped recommended test, treatment, or follow-up
• Did not get needed specialist care
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 9
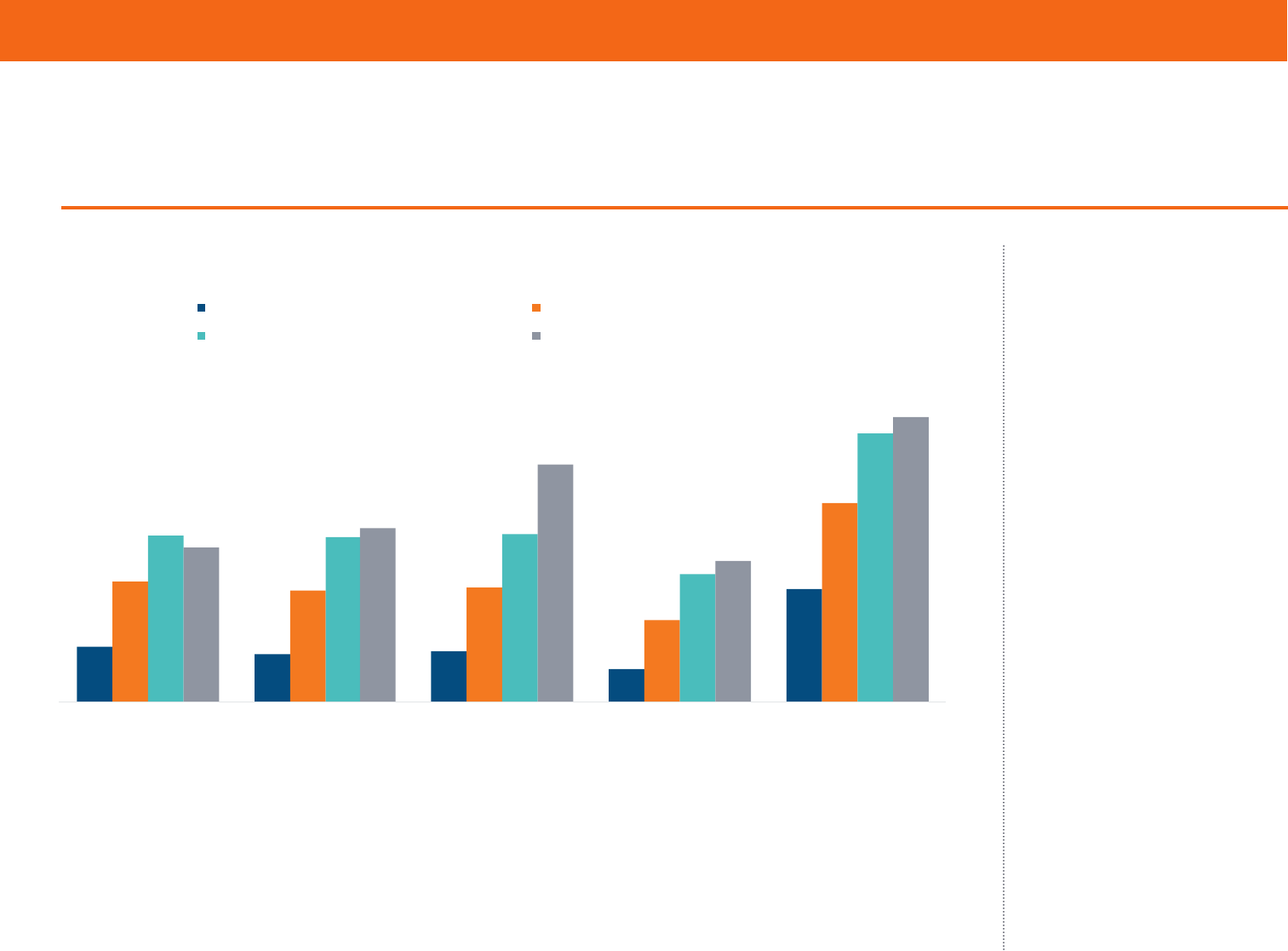
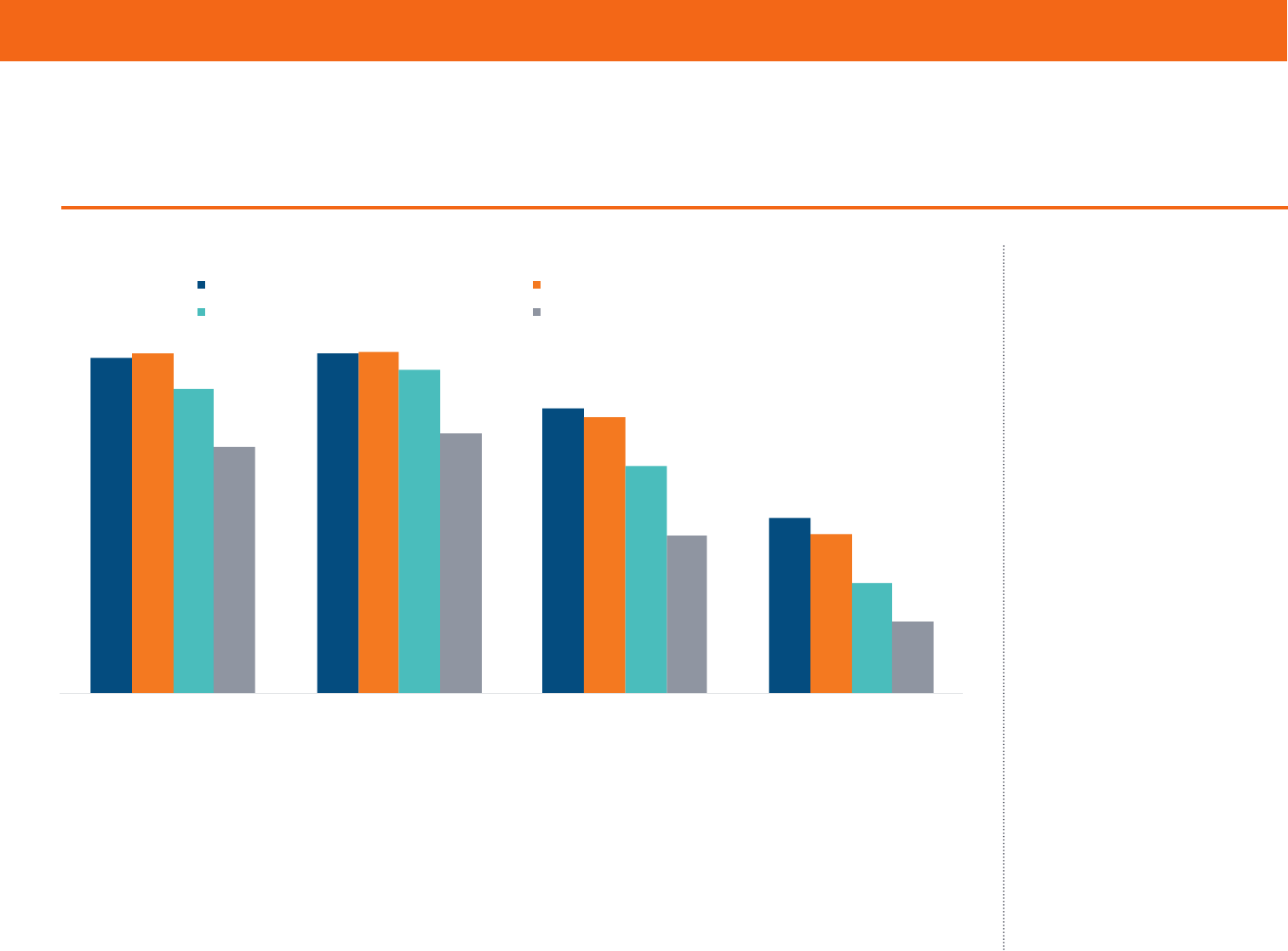
Inadequate Coverage Is Associated with More Cost-Related Problems Getting
Needed Care
The lack of continued
improvement in
overall access to care
nationally reflects the
fact that coverage gains
have plateaued, and
underinsured rates have
climbed. People who
experience any time
uninsured are more likely
than any other group to
delay getting care because
of cost (Table 5). And among
people with coverage
all year, those who were
underinsured reported
cost-related delays in getting
care at nearly double the
rate of those who were not
underinsured.
Notes: * Includes any of the following because of cost: did not ll a prescription; skipped recommended medical test, treatment, or follow-up;
had a medical problem but did not visit doctor or clinic; did not see a specialist when needed. “Underinsured” refers to adults who were insured
all year but experienced one of the following: out-of-pocket costs, excluding premiums, equaled 10% or more of income; out-of-pocket costs,
excluding premiums, equaled 5% or more of income if low-income (<200% of poverty); or deductibles equaled 5% or more of income. “Insured
now, had a coverage gap” refers to adults who were insured at the time of the survey but were uninsured at any point in the 12 months prior to
the survey eld date. “Uninsured now” refers to adults who reported being uninsured at the time of the survey.
Data: Commonwealth Fund Biennial Health Insurance Survey (2018).
Source: Sara R. Collins, Herman K. Bhupal, and Michelle M. Doty, Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and
Shorter Coverage Gaps, But More Underinsured — Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2018 (Commonwealth Fund,
Feb. 2019).
Inadequate Coverage Is Associated with More Cost-Related Problems Getting Needed Care
Notes: * Includes any of the following because of cost: did not fill a prescription; skipped recommended medical test, treatment, or follow-up; had a medical problem but did not visit doctor or clinic;
did not see a specialist when needed. “Underinsured” refers to adults who were insured all year but experienced one of the following: out-of-pocket costs, excluding premiums, equaled 10% or more
of income; out-of-pocket costs, excluding premiums, equaled 5% or more of income if low-income (<200% of poverty); or deductibles equaled 5% or more of income. “Insured now, had a coverage
gap” refers to adults who were insured at the time of the survey but were uninsured at any point in the 12 months prior to the survey field date. “Uninsured now” refers to adults who reported being
uninsured at the time of the survey.
Data: Commonwealth Fund Biennial Health Insurance Survey (2018).
Percent of adults ages 19–64 who had any of four access problems in past year because of cost*
11
10
11
7
23
25
23
24
17
41
35
34
35
27
56
32
36
49
29
59
Did not fill prescription Skipped recommended
test, treatment, or
follow-up
Had a medical p roblem,
did not visit doctor
or clinic
Did not get needed
specialist care
At least one of four
access problems
because of cost
Insured all year, not underinsured Insured all year, underinsured
Insured now, had a coverage gap Uninsured now
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 10
There was modest but
significant improvement
following the ACA’s
coverage expansions in
the proportion of all U.S.
adults who reported having
diculty paying their
medical bills or said they
were paying o medical debt
over time (Table 4). Federal
surveys have found similar
improvements.
8
However,
those gains have stalled.
Data: Commonwealth Fund Biennial Health Insurance Surveys (2005, 2010, 2012, 2014, 2016, 2018).
Source: Sara R. Collins, Herman K. Bhupal, and Michelle M. Doty, Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and
Shorter Coverage Gaps, But More Underinsured — Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2018 (Commonwealth Fund,
Feb. 2019).
Fewer Adults Have Difficulty Paying Their Medical Bills, but the Improvement Has Stalled
Data: Commonwealth Fund Biennial Health Insurance Surveys (2005, 2010, 2012, 2014, 2016, 2018).
34
40
41
35
37
37
2005 2010 2012 2014 2016 2018
Percent of adults ages 19–64 who reported any of the following
medical bill or debt problems in the past year:
• Had problems paying or unable to pay medical bills
• Contacted by a collection agency for unpaid medical bills
• Had to change way of life to pay bills
• Medical bills/debt being paid off over time
Fewer Adults Have Difficulty Paying Their Medical Bills, but the Improvement
Has Stalled
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 11
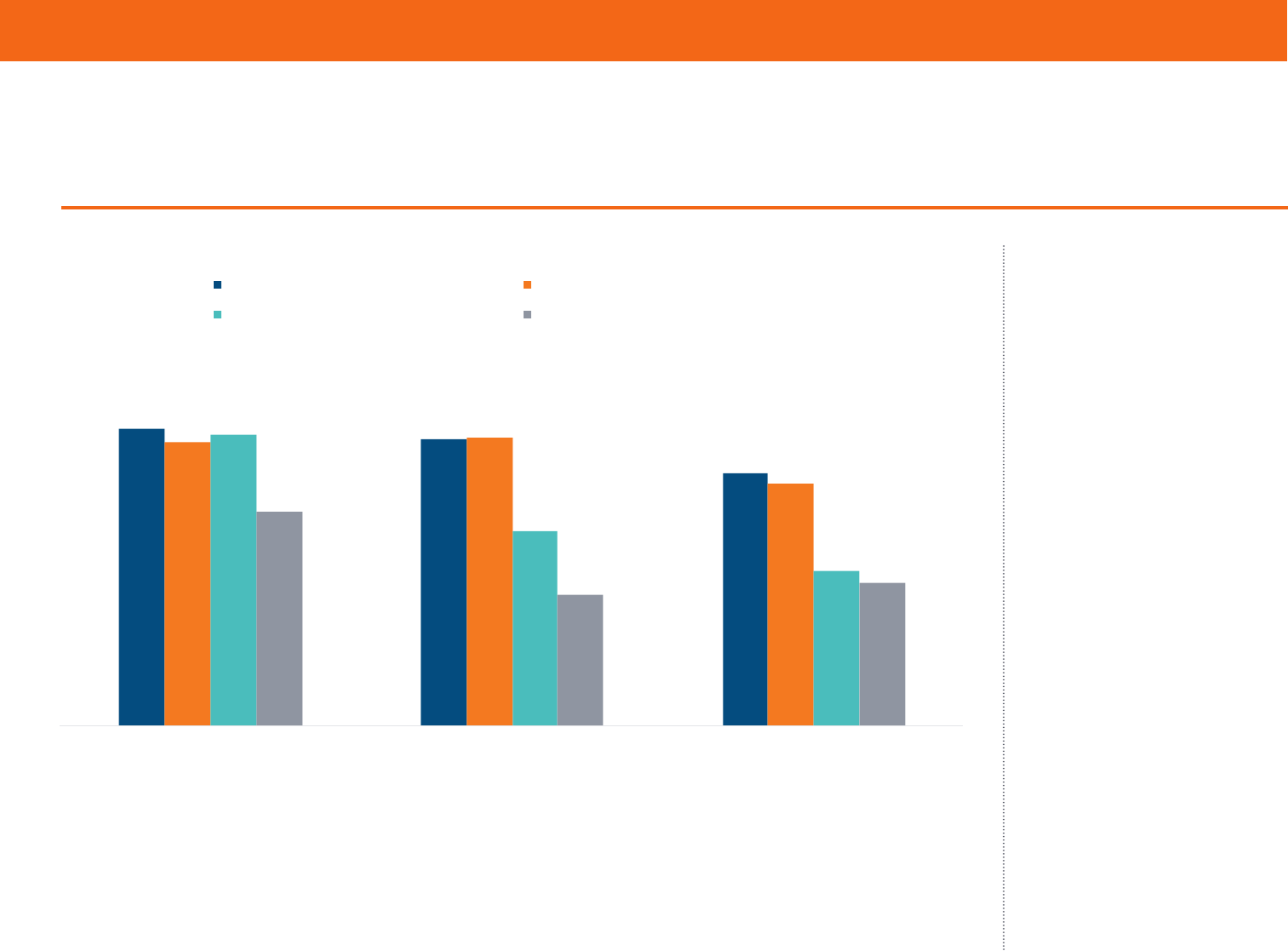
Inadequate insurance
coverage leaves people
exposed to high health care
costs, and these expenses
can quickly turn into
medical debt. More than
half of uninsured adults and
insured adults who have
had a coverage gap reported
that they had had problems
paying medical bills or were
paying o medical debt
over time (Table 6). Among
people who had continuous
insurance coverage, the rate
of medical bill and debt
problems is nearly twice as
high for the underinsured
as it is for people who are
not underinsured.
Notes: * Includes any of the following: had problems paying or unable to pay medical bills; contacted by collection agency for unpaid medical
bills; had to change way of life to pay bills; medical bills/debt being paid over time. “Underinsured” refers to adults who were insured all year but
experienced one of the following: out-of-pocket costs, excluding premiums, equaled 10% or more of income; out-of-pocket costs, excluding
premiums, equaled 5% or more of income if low-income (<200% of poverty); or deductibles equaled 5% or more of income. “Insured now, had a
coverage gap” refers to adults who were insured at the time of the survey but were uninsured at any point in the 12 months prior to the survey
eld date. “Uninsured now” refers to adults who reported being uninsured at the time of the survey.
Data: Commonwealth Fund Biennial Health Insurance Survey (2018).
Source: Sara R. Collins, Herman K. Bhupal, and Michelle M. Doty, Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and
Shorter Coverage Gaps, But More Underinsured — Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2018 (Commonwealth Fund,
Feb. 2019).
13
9
6
16
25
30
19 19
33
47
47
29
26
33
56
40
26
22
26
52
Had problems paying
or unable to p ay
medical bills
Contacted by collection
agency for unpaid
medical bills
Had to change
way of life to pay bills
Medical bills/debt
being paid over time
Any bill problem or
medical debt
Insured all year, not underinsured Insured all year, underinsured
Insured now, had a coverage gap Uninsured now
Inadequate Coverage Is Associated with More Problems Paying Medical Bills
Notes: * Includes any of the following: had problems paying or unable to pay medical bills; contacted by collection agency for unpaid medical bills; had to change way of life to pay bills; medical
bills/debt being paid over time. “Underinsured” refers to adults who were insured all year but experienced one of the following: out-of-pocket costs, excluding premiums, equaled 10% or more of
income; out-of-pocket costs, excluding premiums, equaled 5% or more of income if low-income (<200% of poverty); or deductibles equaled 5% or more of income. “Insured now, had a coverage gap”
refers to adults who were insured at the time of the survey but were uninsured at any point in the 12 months prior to the survey field date. “Uninsured now” refers to adults who reported being
uninsured at the time of the survey.
Data: Commonwealth Fund Biennial Health Insurance Survey (2018).
Percent of adults ages 19–64 who had medical bill or debt problems in past year*
Inadequate Coverage Is Associated with More Problems Paying Medical Bills
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 12
Having continuous
coverage makes a significant
dierence in whether
people have a regular
source of care, get timely
preventive care, or receive
recommended cancer
screenings. Adults with
coverage gaps or those who
were uninsured when they
responded to the survey
were the least likely to have
gotten preventive care and
cancer screenings in the
recommended time frame.
Notes: “Continuously insured” refers to adults who were insured for the full year up to and on the survey eld date. “Underinsured” refers
to adults who were insured all year but experienced one of the following: out-of-pocket costs, excluding premiums, equaled 10% or more of
income; out-of-pocket costs, excluding premiums, equaled 5% or more of income if low-income (<200% of poverty); or deductibles equaled
5% or more of income. “Insured now, had a coverage gap” refers to adults who were insured at the time of the survey but were uninsured at any
point in the 12 months prior to the survey eld date. “Uninsured now” refers to adults who reported being uninsured at the time of the survey.
Respondents were asked if they: had their blood pressure checked within the past two years (in past year if has hypertension or high blood
pressure); had their cholesterol checked in past ve years (in past year if has hypertension, heart disease, or high cholesterol); and had their
seasonal u shot within the past 12 months.
Data: Commonwealth Fund Biennial Health Insurance Survey (2018).
Source: Sara R. Collins, Herman K. Bhupal, and Michelle M. Doty, Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and
Shorter Coverage Gaps, But More Underinsured — Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2018 (Commonwealth Fund,
Feb. 2019).
Continuously Insured Adults, Including Those Underinsured, Are More Likely to Get
Preventive Care
Notes: “Continuously insured” refers to adults who were insured for the full year up to and on the survey field date. “Underinsured” refers to adults who were insured all year but experienced one of
the following: out-of-pocket costs, excluding premiums, equaled 10% or more of income; out-of-pocket costs, excluding premiums, equaled 5% or more of income if low-income (<200% of poverty);
or deductibles equaled 5% or more of income. “Insured now, had a coverage gap” refers to adults who were insured at the time of the survey but were uninsured at any point in the 12 months prior to
the survey field date. “Uninsured now” refers to adults who reported being uninsured at the time of the survey. Respondents were asked if they: had their blood pressure checked within the past two
years (in past year if has hypertension or high blood pressure); had their cholesterol checked in past five years (in past year if has hypertension, heart disease, or high cholesterol); and had their
seasonal flu shot within the past 12 months.
Data: Commonwealth Fund Biennial Health Insurance Survey (2018).
93
94
79
48
94
94
76
44
84
89
63
30
68
72
44
20
Regul ar sou rce
of care
Blood pressure
checked
Cholesterol
checked
Seasonal
flu shot
Insured all year, not underinsured Insured all year, underinsured
Insured now, had a coverage gap Uninsured now
Percent of adults ages 19–64
Continuously Insured Adults, Including Those Underinsured, Are More Likely to Get
Preventive Care
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 13
Being underinsured,
however, does not seem
to reduce the likelihood
of having a usual source
of care or receiving timely
preventive care or cancer
screens — provided a
person has continuous
coverage. This is likely
because the ACA requires
insurers and employers
to cover recommended
preventive care and
cancer screens without
cost-sharing. Even prior
to the ACA, a majority of
employer plans provided
predeductible coverage of
preventive services.
9
Notes: “Continuously insured” refers to adults who were insured for the full year up to and on the survey eld date. “Underinsured” refers
to adults who were insured all year but experienced one of the following: out-of-pocket costs, excluding premiums, equaled 10% or more of
income; out-of-pocket costs, excluding premiums, equaled 5% or more of income if low-income (<200% of poverty); or deductibles equaled
5% or more of income. “Insured now, had a coverage gap” refers to adults who were insured at the time of the survey but were uninsured at any
point in the 12 months prior to the survey eld date. “Uninsured now” refers to adults who reported being uninsured at the time of the survey.
Respondents were asked if they: received a Pap test within the past three years for females ages 21–64, received a mammogram within the
past two years for females ages 40–64, and received a colon cancer screening within the past ve years for adults ages 50–64.
Data: Commonwealth Fund Biennial Health Insurance Survey (2018).
Source: Sara R. Collins, Herman K. Bhupal, and Michelle M. Doty, Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and
Shorter Coverage Gaps, But More Underinsured — Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2018 (Commonwealth Fund,
Feb. 2019).
Continuously Insured Adults, Including Those Underinsured, Are More Likely to Get
Cancer Screenings
73
71
63
70
71
60
72
48
38
53
32
35
Received Pap test Received mammogram Received colon cancer screening
Insured all year, not underinsured Insured all year, underinsured
Insured now, had a coverage gap Uninsured now
Notes: “Continuously insured” refers to adults who were insured for the full year up to and on the survey field date. “Underinsured” refers to adults who were insured all year but experienced one of
the following: out-of-pocket costs, excluding premiums, equaled 10% or more of income; out-of-pocket costs, excluding premiums, equaled 5% or more of income if low-income (<200% of poverty);
or deductibles equaled 5% or more of income. “Insured now, had a coverage gap” refers to adults who were insured at the time of the survey but were uninsured at any point in the 12 months prior to
the survey field date. “Uninsured now” refers to adults who reported being uninsured at the time of the survey. Respondents were asked if they: received a Pap test within the past three years for
females ages 21–64, received a mammogram within the past two years for females ages 40–64, and received a colon cancer screening within the past five years for adults ages 50–64.
Data: Commonwealth Fund Biennial Health Insurance Survey (2018).
Percent of adults ages 19–64
Continuously Insured Adults, Including Those Underinsured, Are More Likely to
Get Cancer Screenings

commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 14
CONCLUSION AND POLICY IMPLICATIONS
U.S. working-age adults are significantly more likely to have health
insurance since the ACA became law in 2010. But the improvement
in uninsured rates has stalled. In addition, more people have health
plans that fail to adequately protect them from health care costs, with
the fastest deterioration in cost protection occurring in the employer
market. The ACA made only minor changes to employer plans, and
the erosion in cost protection has taken a bite out of the progress
made in Americans’ health coverage since the law’s enactment.
Both the federal government and the states, however, have the ability
to extend the law’s coverage gains and improve the cost protection
of both individual-market and employer plans. Here is a short list of
policy options:
Increase Coverage
• Expand Medicaid without restrictions. The 2018 midterm elections
moved as many as five states closer to joining the 32 states that,
along with the District of Columbia, have expanded eligibility
for Medicaid under the ACA.
10
As many as 300,000 people
may ultimately gain coverage as a result.
11
But, encouraged by
the Trump administration, several states are imposing work
requirements on people eligible for Medicaid — a move that
could reverse these coverage gains. So far, the U.S. Department
of Health and Human Services (HHS) has approved similar
work-requirement waivers in seven states and is considering
applications from at least seven more. Arkansas imposed a work
requirement last June, and, to date, more than 18,000 adults have
lost their insurance coverage as a result.
• Ban or place limits on short-term health plans and other insurance
that doesn’t comply with the ACA. The Trump administration
loosened regulations on short-term plans that don’t comply with
the ACA, potentially leaving people who enroll in them exposed
to high costs and insurance fraud. These plans also will draw
healthier people out of the marketplaces, increasing premiums
for those who remain and federal costs of premium subsidies.
Twenty-three states have banned or placed limits on short-term
insurance policies. Some lawmakers have proposed a federal ban.
• Reinsurance, either state or federal. The ACA’s reinsurance
program was eective in lowering marketplace premiums. Aer it
expired in 2017, several states implemented their own reinsurance
programs.
12
Alaska’s program reduced premiums by 20 percent in
2018. These lower costs particularly help people whose incomes
are too high to qualify for ACA premium tax credits. More states
are seeking federal approval to run programs in their states. Several
congressional bills have proposed a federal reinsurance program.
• Reinstate outreach and navigator funding for the 2020 open-
enrollment period. The administration has nearly eliminated
funding for advertising and assistance to help people enroll in
marketplace plans.
13
Research has found that both activities
are eective in increasing enrollment.
14
Some lawmakers have
proposed reinstating this funding.
• Li the 400-percent-of-poverty cap on eligibility for marketplace
tax credits. This action would help people with income exceeding
$100,000 (for a family of four) better aord marketplace plans. The
tax credits work by capping the amount people pay toward their
premiums at 9.86 percent. Liing the cap has a built in phase out:
as income rises, fewer people qualify, since premiums consume an
increasingly smaller share of incomes. RAND researchers estimate
that this policy change would increase enrollment by 2 million
and lower marketplace premiums by as much as 4 percent as
healthier people enroll. It would cost the federal government an
estimated $10 billion annually.
15
Legislation has been introduced
to li the cap.

commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 15
• Make premium contributions for individual market plans fully tax
deductible. People who are self-employed are already allowed to
do this.
16
• Fix the so-called family coverage glitch. People with employer
premium expenses that exceed 9.86 percent of their income
are eligible for marketplace subsidies, which trigger a federal
tax penalty for their employers. There’s a catch: this provision
applies only to single-person policies, leaving many middle-
income families caught in the “family coverage glitch.” Congress
could lower many families’ premiums by pegging unaordable
coverage in employer plans to family policies instead of single
policies.
17
Reduce Coverage Gaps
• Inform the public about their options. People who lose coverage
during the year are eligible for special enrollment periods for
ACA marketplace coverage. Those eligible for Medicaid can sign
up at any time. But research indicates that many people who
lose employer coverage do not use these options.
18
The federal
government, the states, and employers could increase awareness
of insurance options outside the open-enrollment periods
through advertising and education.
• Reduce churn in Medicaid. Research shows that over a two-year
period, one-quarter of Medicaid beneficiaries leave the program
and become uninsured.
19
Many do so because of administrative
barriers.
20
By imposing work requirements, as some states are
doing, this involuntary disenrollment is likely to get worse. To
help people stay continuously covered, the federal government
and the states could consider simplifying and streamlining the
enrollment and reenrollment processes.
• Extend the marketplace open-enrollment period. The current
open-enrollment period lasts just 45 days. Six states that run
their own marketplaces have longer periods, some by as much
as an additional 45 days. Other states, as well as the federal
marketplace, could extend their enrollment periods as well.
Improve Individual-Market Plans’ Cost Protections
• Fund and extend the cost-sharing reduction subsidies. The Trump
administration eliminated payments to insurers for oering
plans with lower deductibles and copayments. Insurers, which
by law must still oer reduced-cost plans, are making up the
lost revenue by raising premiums. But this fix, while benefiting
enrollees who are eligible for premium tax credits, has distorted
both insurer pricing and consumer choice.
21
In addition, it is
unknown whether the administration’s support for the fix
will continue in the future, creating uncertainty for insurers.
22
Congress could reinstate the payments to insurers and consider
making the plans available to people with higher earnings.
• Increase the number of services excluded from the deductible.
Most plans sold in the individual market exclude certain
services from the deductible, such as primary care visits and
certain prescriptions.
23
As the survey data suggest, these types
of exclusions appear to be important in ensuring access to
preventive care among people who have coverage but are
underinsured. In 2016, HHS provided a standardized plan
option for insurers that excluded eight health services —
including mental health and substance-use disorder outpatient
visits and most prescription drugs — from the deductible at the
silver and gold level.
24
The Trump administration eliminated
the option in 2018. Congress could make these exceptions
mandatory for all plans.

commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 16
Improve Employer Plans’ Cost Protections
• Increase the ACA’s minimum level of coverage. Under the ACA,
people in employer plans may become eligible for marketplace
tax credits if the actuarial value of their plan is less than 60
percent, meaning that under 60 percent of health care costs,
on average, are covered. Congress could increase this to the 70
percent standard of silver-level marketplace plans, or even higher.
• Require deductible exclusions. Congress could require employers
to increase the number of services that are covered before someone
meets their deductible. Most employer plans exclude at least
some services from their deductibles.
25
Congress could specify a
minimum set of exclusions for employer plans that might resemble
the standardized-choice options that once existed for ACA plans.
• Refundable tax credits for high out-of-pocket costs. Congress could
make refundable tax credits available to help insured Americans
pay for qualifying out-of-pocket costs that exceed a certain
percentage of their income.
26
• Protect consumers from surprise medical bills. Several states
have passed laws that protect patients and their families from
unexpected medical bills, generally from out-of-network
providers.
27
A bipartisan group of U.S. senators has proposed
federal legislation to protect consumers, including people
enrolled in employer and individual-market plans.
Health care costs are primarily what’s driving growth in premiums
across all health insurance markets. Employers and insurers
have kept premiums down by increasing consumers’ deductibles
and other cost-sharing, which in turn is making more people
underinsured. This means that policy options like the ones we’ve
highlighted above will need to be paired with eorts to slow medical
spending. These could include changing how health care is organized
and providers are paid to achieve greater value for health care dollars
and better health outcomes.
28
The government also could tackle
rising prescription drug costs
29
and use antitrust laws to combat the
growing concentration of insurer and provider markets.
30
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 17
HOW WE CONDUCTED THIS STUDY
The Commonwealth Fund Biennial Health Insurance Survey, 2018, was
conducted by SSRS from June 27 to November 11, 2018. The survey
consisted of telephone interviews in English and Spanish and was conducted
among a random, nationally representative sample of 4,225 adults ages 19
to 64 living in the continental United States. A combination of landline and
cellular phone random-digit dial samples was used to reach people. In all, 725
interviews were conducted with respondents on landline telephones and
3,500 interviews were conducted on cellular phones.
The sample was designed to generalize to the U.S. adult population and to
allow separate analyses of responses of low-income households. Statistical
results are weighted to correct for the stratified sample design, the
overlapping landline and cellular phone sample frames, and disproportionate
nonresponse that might bias results. The data are weighted to the U.S. adult
population by age, sex, race/ethnicity, education, household size, geographic
region, population density, and household telephone use, using the U.S.
Census Bureau’s 2017 Annual Social and Economic Supplement.
The resulting weighted sample is representative of the approximately 193.9
million U.S. adults ages 19 to 64. The survey has an overall margin of sampling
error of +/– 1.9 percentage points at the 95 percent confidence level. The
RDD landline portion of the survey achieved a 8.4 percent response rate and
the RDD cellular phone component achieved a 5.2 percent response rate.
We also report estimates from the 2001, 2003, 2005, 2010, 2012, 2014, and
2016 Commonwealth Fund Biennial Health Insurance Surveys. These surveys
were conducted by Princeton Survey Research Associates International
using the same stratified sampling strategy that was used in 2018, except the
2001, 2003, and 2005 surveys did not include a cellular phone random-digit
dial sample. In 2001, the survey was conducted from April 27 through July
29, 2001, and included 2,829 adults ages 19 to 64; in 2003, the survey was
conducted from September 3, 2003, through January 4, 2004, and included
3,293 adults ages 19 to 64; in 2005, the survey was conducted from August
18, 2005, to January 5, 2006, among 3,352 adults ages 19 to 64; in 2010, the
survey was conducted from July 14 to November 30, 2010, among 3,033
adults ages 19 to 64; in 2012, the survey was conducted from April 26 to
August 19, 2012, among 3,393 adults ages 19 to 64; in 2014, the survey was
conducted from July 22 to December 14, 2014, among 4,251 adults ages 19
to 64; and in 2016, the survey was conducted from July 12 to November 20,
2016, among 4,186 adults ages 19 to 64.
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 18
CHANGES IN U.S. UNINSURED RATES SINCE 2013
Uninsured Rate for Adults Compared to Other Surveys Since 2013
Survey
Preimplementation uninsured rate (%)
[95% CI]
Lowest uninsured rate (%)
[95% CI]
Current uninsured rate (%)
[95% CI]
Commonwealth Fund Biennial Health Insurance Survey
a
19.3% [17.5%–21.3%] 12.0% [10.7%–13.52%] (July–Nov. 2016) 12.4% [11.2%–13.7%]
Commonwealth Fund Aordable Care Act Tracking Survey
b
19.9% [18.5%–21.4%] 12.7% [11.5%–14.0%] (Feb.–Apr. 2016) 15.5% [13.7%–17.5%]
National Health Interview Survey (NHIS) (2016)
c
20.4% [19.7%–21.1.%] 12.4% [11.7%–13.1%] (2016) 12.5% [11.6%–13.4%]
Current Population Survey (CPS)
d
18.3% 11.9% (2016) 12.1%
Gallup Healthways Well-Being Index
e,f
20.8% 13.1% (Q4 2016) 16.3%
Urban Institute Health Reform Monitoring Survey
g
17.4% 9.8% (Q1 2016) 10.8%
Methodological Differences Between Surveys
Survey Population Time Frame Sample Frame Response Rate
Commonwealth Fund Biennial Health
Insurance Survey
U.S. adults ages 19–64 Apr.–Aug. 2012 to June–Nov. 2018 Dual-frame, RDD telephone survey
2012: 22% landline, 19% cell;
2018: 8.4% landline, 5.2% cell
Commonwealth Fund Aordable Care
Act Tracking Survey
U.S. adults ages 19–64 July–Sept. 2013 to Feb.–Mar. 2018 Dual-frame, RDD telephone survey
2013: 20.1%;
2018: 7.5%
National Health Interview Survey
(NHIS) (2016)
h,i
U.S. adults ages 18–64 2013 to Jan.–June 2018 Multistage area probability design 70%
Current Population Survey (CPS)
d
U.S. adults ages 18–64 Mar. 2013–2017
Probability-selected sample; personal and
telephone interviews
j
2018: 85%
k
;
2014: 79.6%
l
Gallup Healthways Well-Being Index
m
U.S. adults ages 18–64 2013 to Oct.–Dec. 2018
Before 2018: dual-frame RDD telephone survey;
2018: address-based sampling frame with web
survey
Urban Institute Health Reform
Monitoring Survey
n
U.S. adults ages 18–64 July–Sept. 2013 to Jan.–Mar. 2018
KnowledgePanel-probability-based internet
panel of 55,000 households
~5%
a
Commonwealth Fund Biennial Health Insurance Survey, Apr.–Aug. 2012, July–Nov. 2016, June–Nov. 2018.
b
Commonwealth Fund Affordable Care Act Tracking Survey, July–Sept. 2013, Feb.–Apr. 2016, Feb.–Mar. 2018.
c
Emily P. Zammitti, Robin A. Cohen, and Michael E. Martinez, Health Insurance Coverage: Early Release of Estimates from the National Health Interview Survey, Jan.–June 2017 (National Center for Health Statistics, Nov. 2017);
and Michael E. Martinez, Emily P. Zammitti, and Robin A. Cohen, Health Insurance Coverage: Early Release of Estimates from the National Health Interview Survey, Jan.–June 2018 (National Center for Health Statistics, Nov. 2018).
d
U.S. Census Bureau, 2013, 2016, and 2017 Current Population Reports; for 2013, see https://www.census.gov/cps/data/cpstablecreator.html.
e
Stephanie Marken, “U.S. Uninsured Rate at 11.4% in Second Quarter,” Gallup News, July 10, 2015.
f
Dan Witters, “U.S. Uninsured Rate Rises to Four-Year High,” Gallup News, Jan. 23, 2019.
g
Jennifer Haley et al., “Adults’ Uninsurance Rates Increased by 2018, Especially in States That Did Not Expand Medicaid — Leaving Gaps in Coverage, Access, and Affordability,” Health Affairs Blog, Sept. 26, 2018.
h
Martinez, Zammitti, and Cohen, Health Insurance Coverage, 2018.
i
National Center for Health Statistics, “About the National Health Interview Survey,” fact sheet (NCHS, last updated Jan. 19, 2019).
j
U.S. Census Bureau, “Current Population Survey (CPS): Methodology,” Census Bureau, n.d.
k
U.S. Census Bureau, “Current Population Survey (CPS): Non-Response Rates,” Census Bureau, n.d.
l
U.S. Census Bureau, “Current Population Survey, 2014 ASEC Technical Documentation,” Census Bureau, 2014.
m
Gallup, “How Does the Gallup National Health and Well-Being Index Work?,” Gallup, n.d.
n
Urban Institute Health Policy Center, “Health Reform Monitoring Survey: HRMS Frequently Asked Questions,” Urban, n.d.
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 19
Table 1. Insurance Status by Demographics, 2018 (base: adults ages 19–64)
Total
(19–64)
Insured
all year
Insured all year,
not underinsured
Insured all year,
underinsured
Insured now, had
a coverage gap
Uninsured
now
Total (millions) 193.9 150.6 106.8 43.8 19.3 24.0
Percent distribution 100.0% 77.7% 55.1% 22.6% 10.0% 12.4%
Unweighted n 4225 3254 2272 982 416 555
Gender
Female 52 78 56 22 11 11
Male 48 77 54 23 9 14
Age
19–34 32 69 48 21 14 17
35–49 30 79 58 21 9 12
50–64 35 84 59 26 7 8
Race/Ethnicity
Non-Hispanic White 59 83 58 25 8 9
Black 12 73 56 18 16 11
Latino 18 62 45 17 14 24
Asian/Pacic Islander 4 81 61 21 8 10
Other/Mixed 5 77 51 26 9 14
Poverty status
Below 133% poverty 25 68 37 31 14 18
133%–249% poverty 19 69 45 24 14 17
250%–399% poverty 19 80 57 23 10 10
400% poverty or more 29 91 75 16 5 3
Below 200% poverty 39 67 39 28 15 18
200% poverty or more 53 86 67 19 7 7
Fair/Poor health status,
or any chronic condition*
50 78 54 24 10 12
Adult work status
Full-time 53 81 59 22 9 10
Part-time 14 67 47 20 16 17
Not currently employed 33 77 52 25 9 14
Employer size**
1–19 employees 23 66 44 21 10 24
20–49 employees 11 79 59 20 9 13
50–99 employees 8 74 57 17 14 13
100 or more employees 56 85 62 22 10 6
NOTES
“Underinsured” refers to
adults who were insured all
year but experienced one of
the following: out-of-pocket
costs, excluding premiums,
equaled 10% or more of
income; out-of-pocket costs,
excluding premiums, equaled
5% or more of income if low-
income (<200% of poverty);
or deductibles equaled 5%
or more of income. “Insured
now, had a coverage gap”
refers to adults who were
insured at the time of the
survey but were uninsured at
any point in the 12 months
prior to the survey eld date.
“Uninsured now” refers to
adults who reported being
uninsured at the time of the
survey.
* At least one of the
following chronic conditions:
hypertension or high
blood pressure; heart
disease; diabetes; asthma,
emphysema, or lung disease;
or high cholesterol.
** Base: Full- and part-time
employed adults ages 19–64.
DATA
Commonwealth Fund
Biennial Health Insurance
Survey (2018).
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 20
Table 2. Insurance Status, 2003–2018 (base: adults ages 19–64)
2003 2005 2010 2012 2014 2016 2018
Total (millions) 172.0 172.5 183.6 183.9 182.8 187.4 193.9
Percent distribution 100% 100% 100% 100% 100% 100% 100%
Unweighted n 3293 3352 3033 3393 4251 4186 4225
Insured all year 74 72 72 70 72 78 78
Insured all year, not underinsured 65 63 56 54 55 56 55
Insured all year, underinsured 9 9 16 16 17 22 23
Insured now, had a coverage gap 9 9 8 10 13 10 10
Uninsured now 17 18 20 19 16 12 12
NOTES
“Underinsured” refers to
adults who were insured all
year but experienced one of
the following: out-of-pocket
costs, excluding premiums,
equaled 10% or more of
income; out-of-pocket costs,
excluding premiums, equaled
5% or more of income if low-
income (<200% of poverty);
or deductibles equaled 5%
or more of income. “Insured
now, had a coverage gap”
refers to adults who were
insured at the time of the
survey but were uninsured at
any point in the 12 months
prior to the survey eld date.
“Uninsured now” refers to
adults who reported being
uninsured at the time of the
survey.
DATA
Commonwealth Fund Biennial
Health Insurance Surveys
(2003, 2005, 2010, 2012,
2014, 2016, 2018).
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 21
Table 3. Uninsured Rate by Demographics, 2003–2018 (base: adults ages 19–64)
2003 2005 2010 2012 2014 2016 2018
Total (millions uninsured) 29.8 31.6 37.1 35.5 28.7 22.6 24.0
Percent distribution 17% 18% 20% 19% 16% 12% 12%
Unweighted n 643 716 590 650 685 520 555
Gender
Female 17 18 20 17 13 11 11
Male 17 18 20 22 19 13 14
Age
19–34 24 26 27 23 19 15 17
35–49 15 19 20 22 17 14 12
50–64 11 10 13 13 11 8 8
Race/Ethnicity
Non-Hispanic White 13 13 15 14 10 7 9
Black 23 19 24 20 18 12 11
Latino 37 48 39 40 34 28 24
Asian/Pacic Islander 14 9 9 8 7 4 10
Other/Mixed 17 18 29 29 22 16 14
Poverty status
Below 133% poverty — — 38 35 26 21 18
133%–249% poverty — — 26 22 19 14 17
250%–399% poverty — — 8 11 11 6 10
400% poverty or more — — 4 5 3 3 3
Below 200% poverty 34 39 36 32 24 19 18
200% poverty or more 7 9 7 9 7 4 7
Fair/Poor health status, or
any chronic condition*
17 22 22 20 15 13 12
Adult work status
Full-time 11 14 12 12 11 9 10
Part-time 26 22 32 26 23 16 17
Not currently employed 26 27 28 27 19 15 14
Employer size**
1–19 employees 28 27 — 25 28 24 24
20–49 employees 17 26 — 30 22 14 13
50–99 employees 14 19 13 12 15 12 13
100 or more employees 7 6 8 9 5 4 6
NOTES
“Uninsured” refers to
adults who reported being
uninsured at the time of the
survey.
— Data not collected or
collected dierently for that
year.
** Base: Full- and part-time
employed adults ages 19–64.
DATA
Commonwealth Fund Biennial
Health Insurance Surveys
(2003, 2005, 2010, 2012,
2014, 2016, 2018).
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 22
Table 4. Cost-Related Access Problems and Medical Bill Problems by Year (base: adults ages 19–64)
Percent Estimated millions
2003 2005 2010 2012 2014 2016 2018 2003 2005 2010 2012 2014 2016 2018
Total (adults ages 19–64)
100% 100% 100% 100% 100% 100% 100% 172.0 172.5 183.6 183.9 182.8 187.4 189.7
Access problems in past year
Went without needed care in past year
because of cost:
Did not ll prescription 23 25 26 27 19 19 19 39 43 48 50 35 36 37
Skipped recommended test,
treatment, or follow-up
19 20 25 27 19 18 19 32 34 47 49 35 34 36
Had a medical problem, did not visit
doctor or clinic
22 24 26 29 23 20 21 38 41 49 53 42 37 40
Did not get needed specialist care 13 17 18 20 13 13 14 22 30 34 37 23 25 27
At least one of four access problems
because of cost
37 37 41 43 36 34 35 63 64 75 80 66 63 68
Delayed or did not get dental care 27 — 38 39 32 31 33 46 — 69 72 58 57 65
Medical bill problems in past year
Had problems paying or unable to pay
medical bills
23 23 29 30 23 23 24 40 39 53 55 43 43 46
Contacted by collection agency 21 21 23 22 20 21 22 35 36 42 41 37 38 42
Contacted by collection agency for
unpaid medical bills
— 13 16 18 15 14 15 — 22 30 32 27 25 30
Contacted by collection agency
because of billing mistake
— 7 5 4 4 5 5 — 11 9 7 8 9 10
Had to change way of life to pay bills 15 14 17 16 14 14 13 26 24 31 29 26 26 26
Any bill problem* — 28 34 34 29 29 29 — 48 62 63 53 53 57
Medical bills/debt being paid o over
time
— 21 24 26 22 24 23 — 37 44 48 40 46 45
Any bill problem or medical debt* — 34 40 41 35 37 37 — 58 73 75 64 70 71
NOTES
— Data not collected for
that year.
* Does not include adults who
reported being contacted by
a collection agency because
of a billing mistake..
DATA
Commonwealth Fund Biennial
Health Insurance Surveys
(2003, 2005, 2010, 2012,
2014, 2016, 2018).
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 23
Table 5. Cost-Related Access Problems and Preventive Care by Insurance Continuity, Insurance Status, and Poverty
(base: adults ages 19–64)
Insurance status Insurance type** Federal poverty level
Total 19–64
Insured all year
Insured all year
Insured now,
had a coverage gap
Uninsured now
Employer
Individual*
Medicaid
Medicare (under
age 65, disabled)
Below 133%
poverty
133%– 249%
poverty
250%– 399%
poverty
400% poverty
or more
Insured all
year, not
underinsured
Insured
all year,
underinsured
Total (millions) 193.9 150.6 106.8 43.8 19.3 24.0 102.6 15.8 22.5 15.8 47.8 37.5 37.4 57.1
Percent distribution 100% 78% 55% 23% 10% 12% 53% 8% 12% 8% 25% 19% 19% 29%
Unweighted n 4225 3254 2272 982 416 555 2016 360 523 479 1212 796 783 1138
Access problems in past year
Went without needed care in past year because of cost:
Did not ll prescription 19 15 11 25 35 32 16 21 22 20 24 22 19 13
Skipped recommended test,
treatment, or follow-up
19 14 10 23 34 36 16 25 14 14 18 25 20 14
Had a medical problem,
did not visit doctor or clinic
21 15 11 24 35 49 16 24 16 14 24 28 23 13
Did not get needed specialist care 14 10 7 17 27 29 11 17 12 12 16 19 15 8
At least one of four access
problems because of cost
35 29 23 41 56 59 31 42 32 32 39 43 38 26
Delayed or did not get dental care 33 28 23 41 49 56 26 38 38 35 39 45 38 21
Preventive care
Regular source of care 89 93 93 94 84 68 92 86 93 96 88 88 88 93
Blood pressure checked in past two years
¥
91 94 94 94 89 72 94 94 89 96 88 89 90 96
Dental exam in past year 60 67 67 67 40 32 72 59 49 40 43 49 61 79
Received mammogram in past two years
(females age 40+)
65 71 71 71 48 32 75 60 55 64 56 48 70 75
Received Pap test in past three years
(females ages 21–64)
70 72 73 70 72 53 77 64 71 58 67 63 72 78
Received colon cancer screening in
past ve years (age 50+)
58 62 63 60 38 35 62 52 51 63 50 51 64 63
Cholesterol checked in past ve years
¥¥
72 78 79 76 63 44 80 70 69 77 63 63 71 87
Seasonal u shot in past year 42 47 48 44 30 20 48 36 39 55 40 36 38 51
Access problems for people with health conditions
Unweighted n 474 276 118 158 ^^ 115 143 ^^ ^^ ^^ 198 125 ^^ ^^
Skipped doses or did not ll a prescription
for medications for the health condition(s)
because of the cost of the medicines^
19 14 10 23 ^^ 45 14 ^^ ^^ ^^ 22 30 ^^ ^^
NOTES
“Underinsured” refers to
adults who were insured all
year but experienced one of
the following: out-of-pocket
costs, excluding premiums,
equaled 10% or more of
income; out-of-pocket costs,
excluding premiums, equaled
5% or more of income if low-
income (<200% of poverty);
or deductibles equaled 5% or
more of income. “Insured now,
had a coverage gap” refers to
adults who were insured at the
time of the survey but were
uninsured at any point in the
12 months prior to the survey
eld date. “Uninsured now”
refers to adults who reported
being uninsured at the time of
the survey.
* Individual includes adults
who are enrolled in either
marketplace plans or
purchased directly o the
marketplace.
** Insurance type at time of
survey.
¥ In past year if respondent
has hypertension or high
blood pressure.
¥¥ In past year if respondent
has hypertension or high
blood pressure, heart disease,
or high cholesterol.
^ Base: Respondents with
at least one of the following
health problems: hypertension
or high blood pressure, heart
disease, diabetes, asthma,
emphysema, lung disease, high
cholesterol, depression, kidney
disease, cancer, or stroke.
^^ Insucient sample.
DATA
Commonwealth Fund
Biennial Health Insurance
Survey (2018).
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 24
Table 6. Medical Bill Problems, by Insurance Continuity, Insurance Status, and Poverty (base: adults ages 19–64)
Insurance status Insurance type** Federal poverty level
Total 19–64
Insured all year
Insured all year
Insured now,
had a coverage gap
Uninsured now
Employer
Individual*
Medicaid
Medicare (under
age 65, disabled)
Below 133%
poverty
133%– 249%
poverty
250%– 399%
poverty
400% poverty
or more
Insured all
year, not
underinsured
Insured
all year,
underinsured
Total (millions) 193.9 150.6 106.8 43.8 19.3 24.0 102.6 15.8 22.5 15.8 47.8 37.5 37.4 57.1
Percent distribution 100% 78% 55% 23% 10% 12% 53% 8% 12% 8% 25% 19% 19% 29%
Unweighted n 4225 3254 2272 982 416 555 2016 360 523 479 1212 796 783 1138
Medical bill problems in past year
Went without needed care in past year because of cost:
Had problems paying or unable to pay
medical bills
24 18 13 30 47 40 19 28 23 35 28 35 28 12
Contacted by collection agency for unpaid
medical bills
15 12 9 19 29 26 12 14 15 29 21 27 14 5
Had to change way of life to pay bills 13 10 6 19 26 22 10 16 11 25 16 20 14 7
Any bill problem 29 24 18 38 52 47 23 35 30 46 36 43 32 14
Medical bills/debt being paid o over time 23 21 16 33 33 26 24 22 19 28 21 30 27 19
Any bill problem or medical debt 37 32 25 47 56 52 32 42 35 53 42 48 40 24
Base: Any medical debt
How much are the medical bills that are
being paid o over time?
Less than $2,000 43 46 51 40 35 36 46 52 36 35 46 40 46 39
$2,000 to less than $4,000 22 23 21 26 18 17 22 24 27 15 20 20 22 27
$4,000 to less than $8,000 17 14 9 21 23 22 18 8 9 18 10 21 16 22
$8,000 to less than $10,000 4 4 3 4 5 7 2 6 9 4 6 5 4 3
$10,000 or more 12 10 11 8 16 18 10 6 17 14 14 11 13 9
Was this for care received in past year or earlier?
Past year 47 50 53 48 38 35 53 54 34 37 38 41 49 57
Earlier year 46 43 42 43 49 58 39 38 63 55 56 51 39 38
Both 7 6 5 9 11 7 8 5 1 8 5 8 11 5
Were these bills for someone who was insured
at the time the care was provided or was the
person uninsured then?
Insured at time care was provided 65 77 77 79 42 30 81 73 45 63 49 55 74 86
Uninsured at time care was provided 28 16 15 17 46 64 13 19 47 29 43 37 21 7
NOTES
“Underinsured” refers to
adults who were insured all
year but experienced one of
the following: out-of-pocket
costs, excluding premiums,
equaled 10% or more of
income; out-of-pocket costs,
excluding premiums, equaled
5% or more of income if low-
income (<200% of poverty);
or deductibles equaled 5%
or more of income. “Insured
now, had a coverage gap”
refers to adults who were
insured at the time of the
survey but were uninsured at
any point in the 12 months
prior to the survey eld date.
“Uninsured now” refers to
adults who reported being
uninsured at the time of the
survey.
* Individual includes adults
who are enrolled in either
marketplace plans or
purchased directly o the
marketplace.
** Insurance type at time of
survey.
DATA
Commonwealth Fund
Biennial Health Insurance
Survey (2018).

commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 25
NOTES
1. Analysis of the 2018 U.S. Current Population Survey by Ougni Chakraborty
and Sherry Glied of New York University for the Commonwealth Fund.
2. One of the ACA’s most notable provisions aimed at employers was the
so-called employer mandate — the requirement that large firms oer aordable
coverage to full-time employees or pay penalties.
3. Princeton Survey Research Associates International conducted the prior-year
Biennial Surveys analyzed in this brief.
4. Centers for Medicare and Medicaid Services, “Eectuated Enrollment for the
First Half of 2018,” fact sheet, Nov. 28, 2018.
5. Sara R. Collins and David C. Radley, The Cost of Employer Insurance Is a
Growing Burden for Middle-Income Families (Commonwealth Fund, Dec. 2018).
6. Benjamin D. Sommers et al.,“Three-Year Impacts of the Aordable Care Act:
Improved Medical Care and Health Among Low-Income Adults,” Health Aairs
Web First, published online May 17, 2017; and Munira Z. Gunja, Sara R. Collins,
and Herman K. Bhupal, Is the Aordable Care Act Helping Consumers Get Health
Care? Findings from the Commonwealth Fund Aordable Care Act Tracking
Survey, March–June 2017 (Commonwealth Fund, Dec. 2017).
7. Tainya C. Clarke, Tina Norris, and Jeannine S. Schiller, Early Release of Selected
Estimates Based on Data From the 2016 National Health Interview Survey
(National Center for Health Statistics, May 2017).
8. Robin A. Cohen and Jeannine S. Schiller, Problems Paying Medical Bills Among
Persons Under Age 65: Early Release of Estimates from the National Health
Interview Survey, 2011–June 2016 (National Center for Health Statistics, Dec.
2015).
9. “Interim Final Rules for Group Health Plans and Health Insurance Issuers
Relating to Coverage of Preventive Services Under the Patient Protection and
Aordable Care Act,” Federal Register 75, no. 137 (July 19, 2010): 41726–60.
10. In three states — Idaho, Nebraska, and Utah — voters approved ballot
initiatives to expand eligibility for Medicaid; Kansas elected a Democratic
governor who has pledged to expand; Maine’s newly elected Democratic
governor is expanding Medicaid one year aer voters approved a ballot initiative
to expand. See Donald Moulds et al., “The Midterm Election Results Have Big
Implications for Health Care,” To the Point (blog), Commonwealth Fund, Nov. 7.
2018.
11. Matthew Buettgens, The Implications of Medicaid Expansion in the Remaining
States: 2018 Update (Urban Institute, May 2018); and Rachel Garfield, Anthony
Damico, and Kendal Orgera, The Coverage Gap: Uninsured Poor Adults in States
that Do Not Expand Medicaid (Henry J. Kaiser Family Foundation, June 2018).
12. American Academy of Actuaries, Drivers of 2016 Health Insurance Premium
Changes (AAA, Aug. 2015).
13. Sara R. Collins, “Consumers Shopping for Health Plans Are Le in the Dark by
Trump Administration,” To the Point (blog), Commonwealth Fund, July 19, 2018.
14. Sara R. Collins, Munira Z. Gunja, and Michelle M. Doty, Following the ACA
Repeal-and-Replace Eort, Where Does the U.S. Stand on Insurance Coverage?
Findings from the Commonwealth Fund Aordable Care Act Tracking Survey,
March–June 2017 (Commonwealth Fund, Sept. 2017).
15. Jodi Liu and Christine Eibner, Expanding Enrollment Without the
Individual Mandate: Options to Bring More People into the Individual Market
(Commonwealth Fund, Aug. 2018).
16. Timothy S. Jost, “Fixing Our Most Pressing Health Insurance Problems: A
Bipartisan Path Forward,” To the Point (blog), Commonwealth Fund, July 13,
2017.
17. Christine Eibner, Sarah Nowak, and Jodi Liu, Hillary Clinton’s Health Care Re-
form Proposals: Anticipated Eects on Insurance Coverage, Out-of-Pocket Costs,
and the Federal Deficit (Commonwealth Fund, Sept. 2016).

commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 26
18. Matthew Buettgens, Stan Dorn, and Hannah Recht, More Than 10 Million
Uninsured Could Obtain Marketplace Coverage Through Special Enrollment
Periods (Robert Wood Johnson Foundation and Urban Institute, Nov. 2015).
19. Sara R. Collins, Sherry A. Glied, and Adlan Jackson, The Potential Implications
of Work Requirements for the Insurance Coverage of Medicaid Beneficiaries: The
Case of Kentucky (Commonwealth Fund, Oct. 2018).
20. Benjamin D. Sommers, “Loss of Health Insurance Among Non-Elderly Adults
in Medicaid,” Journal of General Internal Medicine 24, no. 1 (Jan. 2009): 1–7.
21. Christina Cousart, How Elimination of Cost-Sharing Reduction Payments
Changed Consumer Enrollment in State-Based Marketplaces (National Academy
for State Health Policy, March 20, 2018).
22. Centers for Medicare and Medicaid Services, “CMS Issues the Proposed
Payment Notice for the 2020 Coverage Year,” news release, Jan. 17, 2019.
23. Munira Z. Gunja, Sara R. Collins, and Sophie Beutel, How Deductible
Exclusions in Marketplace Plans Improve Access to Many Health Care Services
(Commonwealth Fund, Mar. 2016).
24. Sara R. Collins, “The Trump Administration’s New Marketplace Rules:
Regulatory Simplification or More Complexity for Consumers?” To the Point
(blog), Commonwealth Fund, Apr. 13, 2018.
25. Jon R. Gabel et al., Consumer Cost-Sharing in Marketplace vs. Employer Health
Insurance Plans, 2015 (Commonwealth Fund, Dec. 2015).
26. Christine Eibner, Sarah Nowak, and Jodi Liu, Hillary Clinton’s Health Care
Reform Proposals: Anticipated Eects on Insurance Coverage, Out-of-Pocket
Costs, and the Federal Deficit (Commonwealth Fund, Sept. 2016).
27. Jack Hoadley, Kevin Lucia, and Maanasa Kona, “State Eorts to Protect
Consumers from Balance Billing,” To the Point (blog), Commonwealth Fund, Jan.
18, 2019.
28. David Blumenthal, Lovisa Gustafsson, and Shawn Bishop, “To Control
Health Care Costs, U.S. Employers Should Form Purchasing Alliances,” Harvard
Business Review, published online Nov. 2, 2018.
29. Henry Waxman et al., Getting to the Root of High Prescription Drug Prices
(Commonwealth Fund, July 2017).
30. Richard M. Scheer, Daniel R. Arnold, and Christopher M. Whaley,
“Consolidation Trends in California’s Health Care System: Impacts on ACA
Premiums and Outpatient Visit Prices,” Health Aairs 37, no. 9 (Sept. 2018):
1409–16.
commonwealthfund.org Survey Brief, February 2019
Health Insurance Coverage Eight Years After the ACA: Fewer Uninsured Americans and Shorter Coverage Gaps, But More Underinsured 27
ABOUT THE AUTHORS
Sara R. Collins, Ph.D., is vice president for Health Care Coverage and
Access at the Commonwealth Fund. An economist, Dr. Collins joined the
Fund in 2002 and has led the Fund’s national program on health insurance
since 2005. Since joining the Fund, she has led several national surveys on
health insurance and authored numerous reports, issue briefs, and journal
articles on health insurance coverage and policy. She has provided invited
testimony before several Congressional committees and subcommittees.
Prior to joining the Fund, Dr. Collins was associate director/senior research
associate at the New York Academy of Medicine. Earlier in her career, she
was an associate editor at U.S. News & World Report, a senior economist
at Health Economics Research, and a senior health policy analyst in the
New York City Oce of the Public Advocate. Dr. Collins holds a Ph.D. in
economics from George Washington University.
Herman K. Bhupal is program associate in the Health Care Coverage
and Access program at the Commonwealth Fund, joining the sta in
June 2017. She is responsible for providing daily support for the program,
with responsibilities ranging from daily administrative and grants
management tasks to writing and research. Prior to joining the Fund,
Ms. Bhupal was an associate at PwC Strategy&, where she served several
health care clients in a strategy consulting role. She graduated with a B.A.
in economics with honors from Harvard University in May 2016.
Michelle McEvoy Doty, Ph.D., is vice president of survey research
and evaluation for the Commonwealth Fund. She has authored
numerous publications on cross-national comparisons of health system
performance, access to quality health care among vulnerable populations,
and the extent to which lack of health insurance contributes to inequities
in quality of care. Dr. Doty holds an M.P.H. and a Ph.D. in public health
from the University of California, Los Angeles.
ACKNOWLEDGMENTS
The authors thank Robyn Rapoport, Rob Manley, and Erin Czyzewicz
of SSRS, and David Blumenthal, Donald Moulds, Kathleen Regan,
Chris Hollander, Deborah Lorber, Paul Frame, Jen Wilson, Susan
Hayes, Corinne Lewis, and Arnav Shah of the Commonwealth Fund.
Editorial support was provided by Christopher Hollander.
For more information about this brief, please contact:
Sara R. Collins, Ph.D.
Vice President, Health Care Coverage and Access
The Commonwealth Fund
srccmwf.org

About the Commonwealth Fund
The mission of the Commonwealth Fund is to
promote a high-performing health care system
that achieves better access, improved quality, and
greater efficiency, particularly for society’s most
vulnerable, including low-income people, the
uninsured, and people of color. Support for this
research was provided by the Commonwealth Fund.
The views presented here are those of the authors
and not necessarily those of the Commonwealth
Fund or its directors, officers, or staff.
